Generic Drug Failure: Why Some Pills Don't Work and What to Do
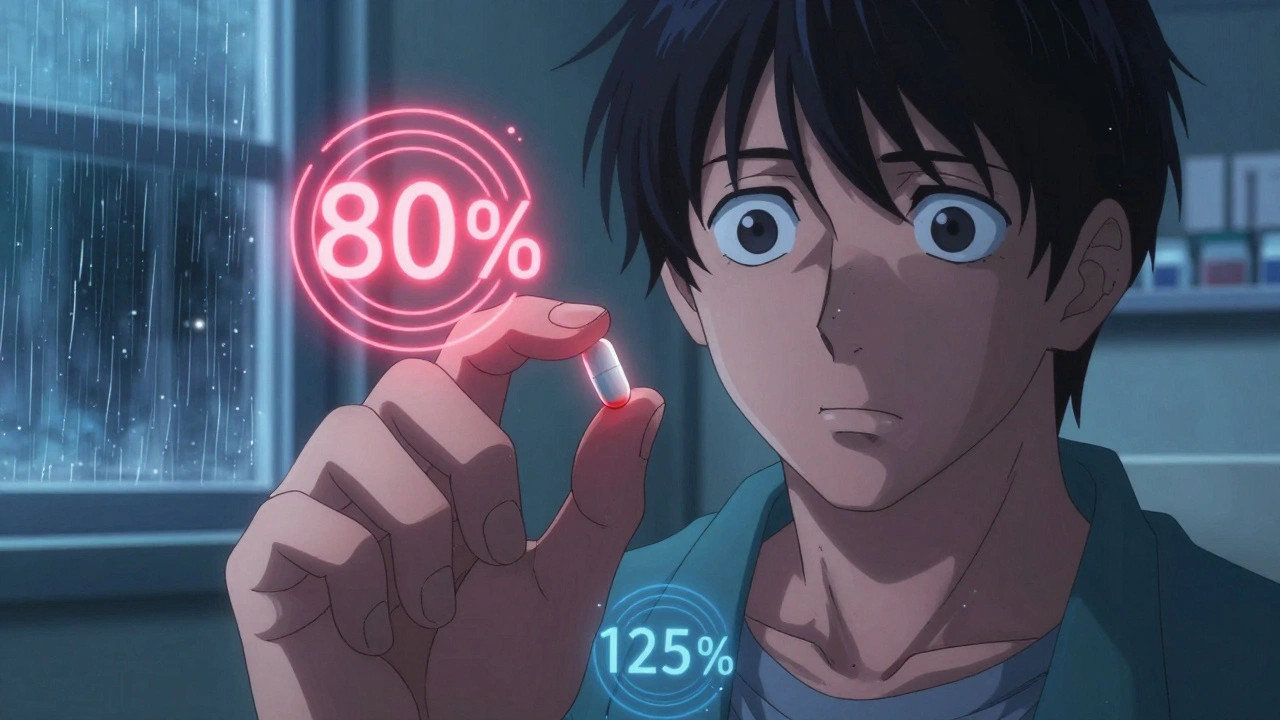
When a generic drug failure, the situation where a generic medication doesn’t produce the expected clinical effect despite being labeled as bioequivalent. Also known as therapeutic failure, it’s not a myth—it’s a documented issue that affects thousands of patients every year. You take your generic blood pressure pill, your thyroid med, or your antidepressant, and suddenly it’s not working like it used to. Your symptoms come back. Your numbers shift. Your doctor says it’s the same drug—so why does it feel different?
The answer isn’t always about the active ingredient. The real problem often hides in the excipients, inactive ingredients like fillers, dyes, and binders that help form the pill but can trigger reactions or alter how the drug is absorbed. One person might tolerate the cornstarch in one brand but react to the lactose in another. Another might find their levothyroxine works perfectly until they switch to a generic made in India instead of the U.S.—not because the active ingredient changed, but because the coating, the particle size, or the manufacturing process did. These tiny differences matter, especially for drugs with a narrow therapeutic index, medications where even small changes in blood levels can cause serious harm or treatment failure like warfarin, lithium, or phenytoin.
And then there’s the reporting gap. Most patients don’t know how to report a generic drug failure, when a generic medication doesn’t work as expected, even though it meets FDA bioequivalence standards to the FDA. They assume it’s just their body changing. But if you don’t report it, regulators never see the pattern. That’s why adverse event reporting, the process of submitting details about unexpected side effects or treatment failures to drug safety agencies matters. Your report could help identify a faulty batch, a problematic manufacturer, or a bioequivalence loophole.
It’s not about trusting or distrusting generics. It’s about knowing they’re not all the same. Some are made with tighter controls. Some use different manufacturing techniques that affect how fast the drug dissolves. And some—though rare—have ingredients that interfere with absorption. That’s why switching brands without telling your doctor can be risky. That’s why tracking your pill’s shape, color, and imprint matters. That’s why keeping a log of when symptoms return after a switch can save your health.
Below, you’ll find real stories and science-backed guides on what to watch for, how to compare manufacturers, when to demand consistency, and how to speak up when something feels off. You’re not imagining it. And you don’t have to accept it.