Barrett's Esophagus: Risks, Monitoring, and Medication Safety
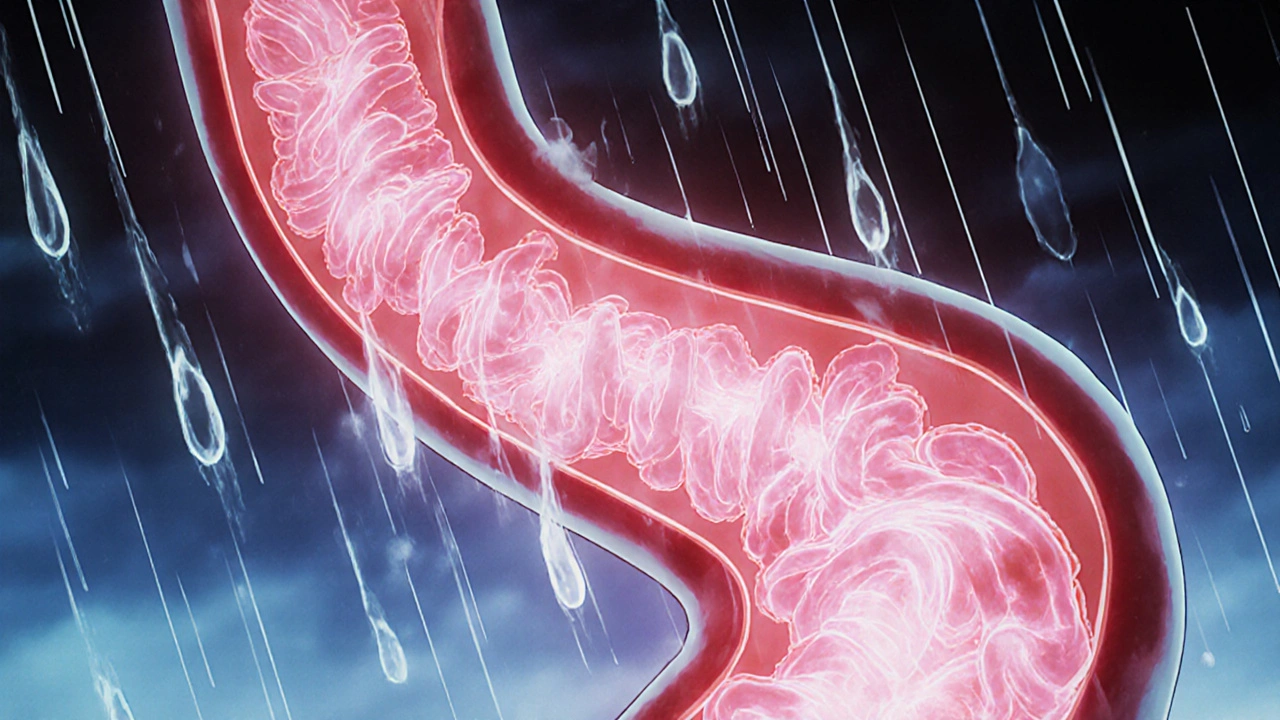
When chronic acid reflux turns the lining of your esophagus into something that looks more like the intestine, you may have Barrett's esophagus, a condition where the esophagus changes due to long-term exposure to stomach acid, raising the risk of esophageal cancer. Also known as Barrett’s syndrome, it doesn’t cause symptoms on its own—but it’s a silent warning sign that your GERD has been running unchecked for years. This isn’t just heartburn you can ignore. If left unmanaged, the cell changes in Barrett’s can slowly become precancerous, and eventually, cancer. The good news? Most people with it never develop cancer—but you need to know what to watch for and how to protect yourself.
Barrett’s esophagus is closely tied to GERD, gastroesophageal reflux disease, a condition where stomach acid flows back into the esophagus frequently, damaging the lining over time. It’s not caused by spicy food alone—it’s about frequency and duration. People who’ve had daily heartburn for over 10 years are at highest risk. But here’s what many don’t realize: some medications used to treat GERD can interact with other drugs you’re taking. For example, if you’re on warfarin, a blood thinner used to prevent clots, often prescribed for atrial fibrillation or after valve replacement, switching generic brands can affect your INR levels, which could mess with your bleeding risk. And if you’re taking levothyroxine, a thyroid hormone replacement that must be taken on an empty stomach for full absorption, fiber supplements or antacids can block it. These aren’t just side effects—they’re real safety issues that can change your health outcome.
Monitoring is key. Regular endoscopies are the standard to check for cell changes, but what you do at home matters too. Avoid lying down after meals. Cut back on alcohol and caffeine. Watch your weight. And if you’re using NSAIDs for joint pain, know that they can worsen stomach lining damage and increase bleeding risk—especially if you already have Barrett’s. The posts below cover exactly these connections: how drug timing, generic switches, and even fiber supplements can interfere with your treatment. You’ll find real advice on avoiding dangerous interactions, spotting early warning signs, and working with your doctor to stay safe. This isn’t just about managing symptoms—it’s about preventing cancer before it starts.