Antibiotic Potency: What Makes Some Antibiotics Stronger Than Others
When we talk about antibiotic potency, how effectively an antibiotic kills or stops bacteria at a given dose. Also known as antibiotic effectiveness, it’s not just about how strong the drug sounds—it’s about how well it works against the specific bacteria causing your infection. A high-potency antibiotic doesn’t always mean better results. Sometimes, a lower-potency drug is the smarter choice if it targets the bug precisely and causes fewer side effects.
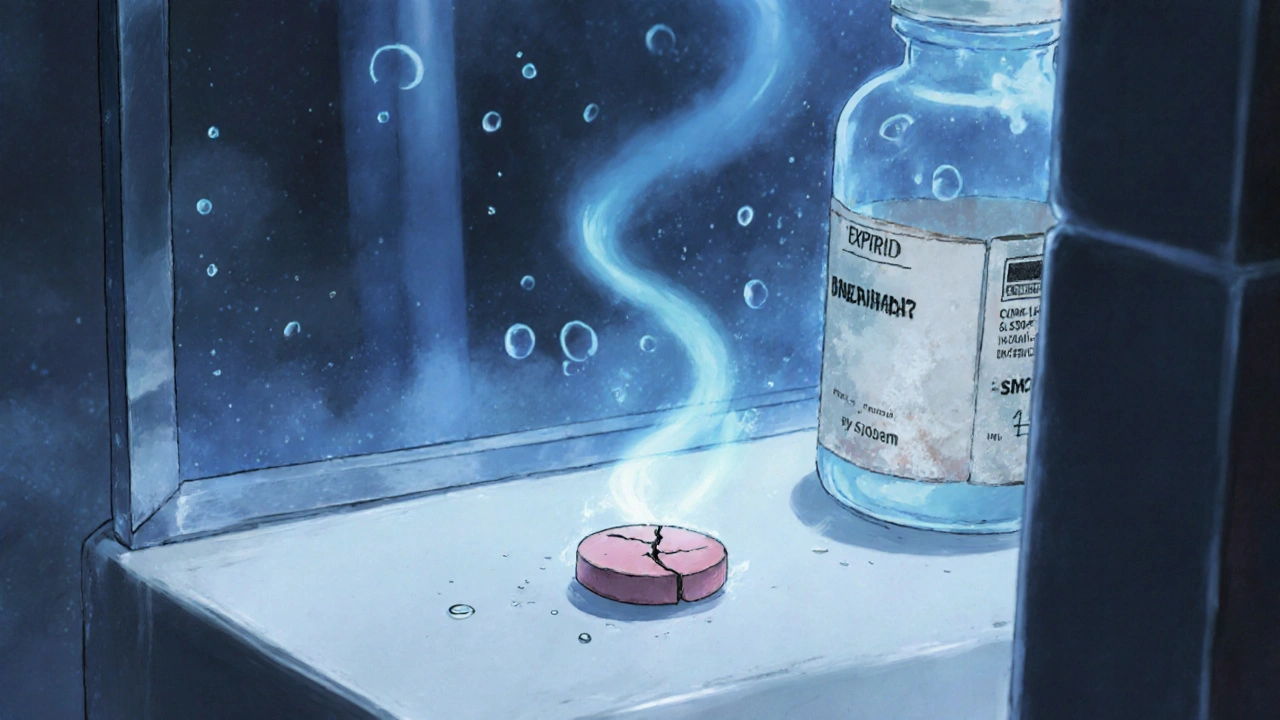
Bacterial resistance, the ability of bacteria to survive exposure to antibiotics that once killed them is the biggest reason potency matters. Over time, some bacteria evolve defenses—like enzymes that break down penicillin or pumps that flush out drugs before they can act. That’s why antibiotic class, the group a drug belongs to based on how it works, like penicillins, cephalosporins, or fluoroquinolones is just as important as strength. A drug in one class might be weak against a certain bug, while another class, even if less potent overall, crushes it.
Antibiotic potency also depends on antibiotic dosage, the amount and frequency of the drug given to reach the level needed to kill bacteria without harming the patient. Too little, and the infection hangs on. Too much, and you risk side effects or fuel resistance. Doctors don’t just pick the strongest drug—they pick the right one for the job, the right dose for your body, and the right duration to avoid creating superbugs.
Some antibiotics kill bacteria outright (bactericidal), others just stop them from multiplying (bacteriostatic). That difference changes how they’re used. For a fast-spreading infection like sepsis, you need a bactericidal drug with high potency. For a stubborn, slow infection like a bone infection, a lower-potency but long-lasting option might work better. It’s not about brute force—it’s about precision.
And potency isn’t just about the drug itself. Where it goes in your body matters. Some antibiotics don’t reach the skin well. Others can’t cross into the brain or prostate. That’s why a drug that’s powerful in a lab might fail in your body. Your doctor has to match the drug’s travel range to the infection’s location.
What you’ll find below are real-world examples of how antibiotic potency plays out in practice—from why clindamycin works for acne but not every infection, to how clavulanic acid boosts amoxicillin to fight resistant bugs, to why some people get no relief from one antibiotic but recover quickly on another. These aren’t theoretical discussions. They’re stories from patients, doctors, and studies showing how potency, resistance, and smart prescribing shape outcomes every day.