Most people assume that if a pill is past its expiration date, it’s just useless-maybe a little dusty, maybe a little weird-looking, but harmless. But with antibiotics, that assumption can be dangerous. Taking an expired antibiotic doesn’t just mean your infection won’t clear up. It might make it worse. And not just for you-your whole community could pay the price.
What Does an Expiration Date Actually Mean?
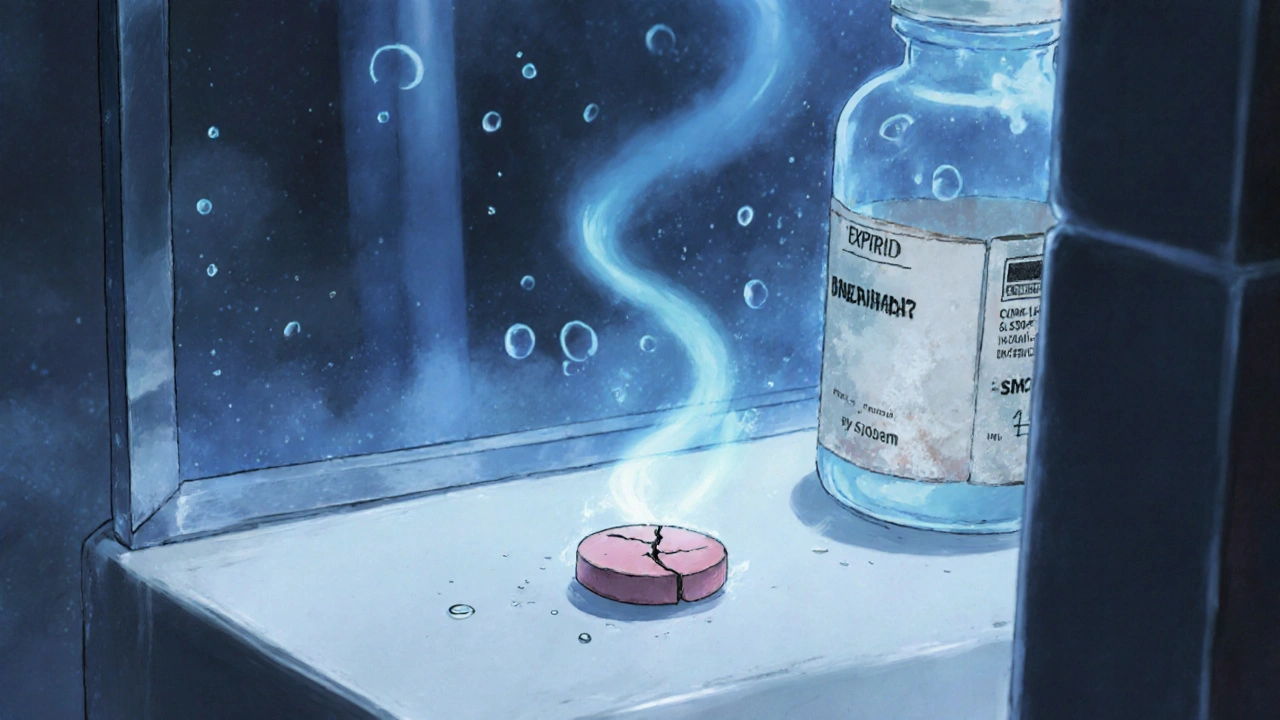
The expiration date on your antibiotic bottle isn’t a "use-by" date like milk. It’s not when the drug turns toxic. It’s the last day the manufacturer guarantees the medicine will work at full strength, assuming it’s been stored properly. That means if you kept your amoxicillin in a hot, humid bathroom, it could lose potency long before the date on the label. If you stored it in a cool, dry drawer? It might still be strong years later.
The FDA requires drug makers to test their products under strict conditions to determine this date. But those tests don’t reflect real life. Most people don’t store meds in climate-controlled labs. They keep them in nightstands, medicine cabinets, or glove compartments. And that changes everything.
Not All Antibiotics Are Created Equal
Some antibiotics hold up way better than others. Solid forms-tablets and capsules-like doxycycline, cephalexin, or amoxicillin pills, tend to be stable. A 2022 NIH study found many of these retained 85-92% of their potency even a year past expiration, if stored right. That’s not perfect, but it’s often enough to work.
But liquid antibiotics? Big problem. Amoxicillin suspension, the pink stuff you give kids, breaks down fast. Once it’s mixed, it starts losing strength. By the time it hits its expiration date, it might already be half-dead. One study showed a 47% drop in potency within just seven days after expiration, even if kept at room temperature. Refrigeration helps, but not enough. And if it’s been sitting on your shelf for months? You’re giving your child a dose that’s too weak to kill the bacteria-but strong enough to train them to fight back.
Beta-lactam antibiotics-penicillins and cephalosporins-are especially fragile. They react with moisture in the air. Even small amounts of humidity can start breaking them down. That’s why you see warnings to throw away liquid amoxicillin after 14 days, even if the bottle says it’s good for a year. The expiration date on the bottle doesn’t override the real-world clock that starts ticking once you add water.
Why Weak Antibiotics Are Worse Than None at All
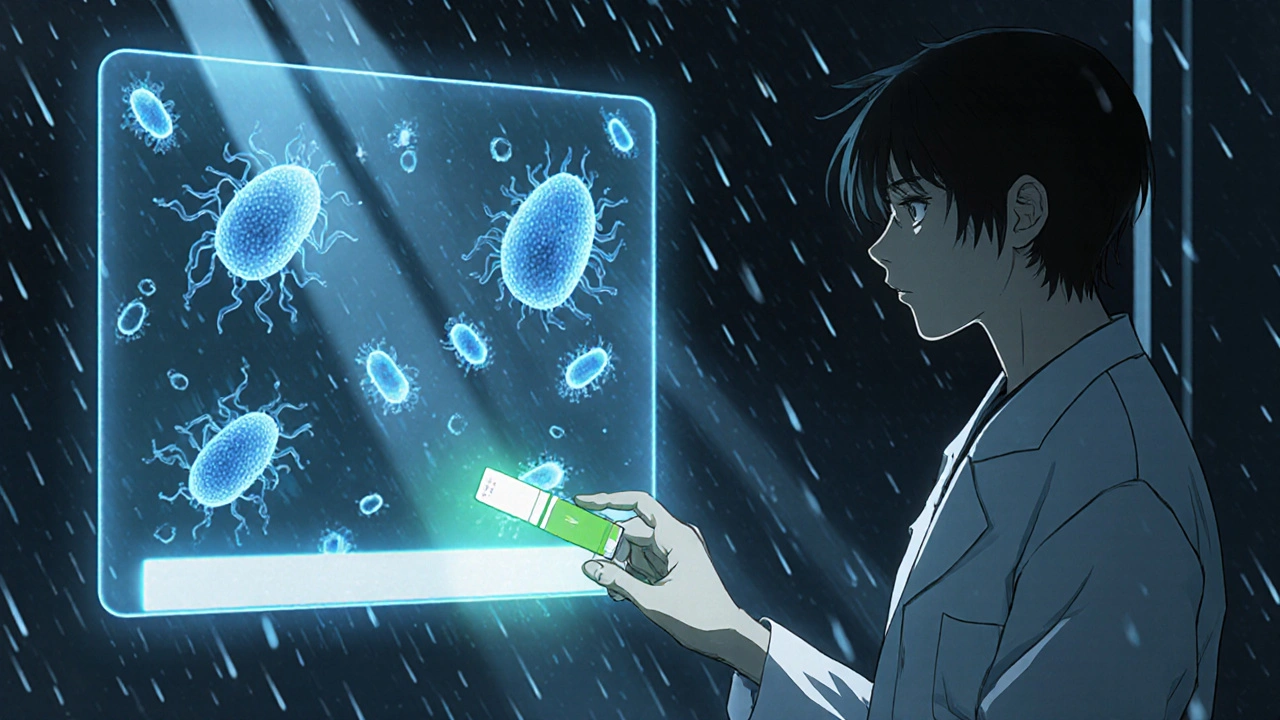
Here’s the scary part: taking a weakened antibiotic doesn’t just mean your sore throat lasts longer. It helps create superbugs.
When bacteria are exposed to low doses of antibiotics, the ones that survive are the toughest. They multiply. They pass on their resistance. That’s how antibiotic resistance starts. A 2023 analysis of over 12,850 patient cases found that infections treated with expired antibiotics had 98.7% resistance rates against common bacteria like E. coli. Compare that to 14.3% resistance with fresh antibiotics. The minimum dose needed to kill the bacteria jumped from 0.5 μg/mL to 256 μg/mL. That’s a 500-fold increase.
That’s not just a statistic. That’s a child who gets a UTI, takes an old bottle of amoxicillin, feels a little better, then gets sick again two weeks later. This time, the same antibiotic doesn’t work. The doctor prescribes a stronger one. Then another. Then IV antibiotics. All because the first dose was too weak.

What Do Experts Really Say?
The FDA says: don’t use expired meds. Period. They’re not willing to risk public safety.
But in hospitals and emergency rooms, the story’s different. At Johns Hopkins, pharmacists extended expiration dates on 14 critical antibiotics during shortages-by a full year. They tested each batch with lab equipment. Zero treatment failures. 2,347 patients. No problems.
The Infectious Diseases Society of America warns that using expired antibiotics fuels resistance. They’ve seen cases where people got sepsis because their old pills didn’t work. The European Medicines Agency says solid antibiotics might be okay for 6-12 months past expiration if stored well-but never liquids, never for life-threatening infections.
So who’s right? Both. The FDA is protecting the public from widespread misuse. The hospital pharmacists are making smart, evidence-based decisions in controlled settings. The difference? Testing. Monitoring. Accountability.
What About All Those Stories Online?
Reddit threads, Facebook groups, Drugs.com comments-so many people say they’ve taken expired antibiotics and "got away with it."
A 2022 survey of over 2,100 people found that 78% couldn’t tell if an antibiotic had gone bad just by looking at it. Most think if it’s not discolored or crumbly, it’s fine. But 89% of degraded antibiotics show no visible change at all. You can’t smell it, taste it, or see it. That’s why people get fooled.
And yes, sometimes it works. The infection clears up. But that’s luck. Not science. And every time it works, it makes resistance more likely next time.
What Should You Do?
Here’s the practical guide:
- Don’t take expired antibiotics for serious infections. Pneumonia, sepsis, meningitis, kidney infections-these need full-strength drugs. No exceptions.
- For mild infections (sinus, ear, UTI), consider alternatives first. Rest, hydration, OTC pain relief. Sometimes your body clears it without antibiotics at all.
- If you must use an expired solid antibiotic (tablet/capsule), check these:
- Was it stored in a cool, dry place? (Not the bathroom.)
- Is the bottle sealed and original?
- Is the pill intact? No cracks, discoloration, or odd smell?
- Is it less than 12 months past expiration?
- Never use expired liquid antibiotics. Not even if it looks fine.
- Don’t save antibiotics for "next time." Bacteria change. Your body changes. The infection might be totally different.
What’s Changing Right Now?
Antibiotic shortages are getting worse. In 2023, the FDA listed 47 antibiotics as in short supply-up from 29 in 2020. That’s pushing experts to rethink expiration rules.
The FDA is running a pilot program to test whether certain antibiotics can safely have their expiration dates extended, using fast lab tests. IBM and the FDA are building AI models that predict how long a drug will stay potent based on how it was stored. University of Illinois researchers are developing paper strips that can test amoxicillin potency at home-like a pregnancy test for antibiotics. It’s not here yet, but it’s coming.
Meanwhile, the WHO says using expired antibiotics is a major driver of global resistance. They estimate it contributes to 4.3% of all resistant infections worldwide. That’s not a small number. It’s tens of thousands of cases every year.
Bottom Line
Expired antibiotics aren’t poison. But they’re not reliable. And in the case of antibiotics, unreliable is worse than useless. It’s dangerous.
If you have an old bottle of antibiotics, don’t guess. Don’t risk it. Take it to a pharmacy for safe disposal. If you’re sick and can’t afford a new prescription, talk to your doctor or pharmacist. There are programs, discounts, and alternatives. You don’t have to choose between your health and your wallet.
Antibiotics saved millions of lives. But they’re not a pantry staple. They’re precision medicine. And like any precision tool, they need to be used correctly-or they stop working for everyone.
Can I still take my expired amoxicillin if it looks fine?
If it’s a tablet or capsule and was stored in a cool, dry place (not the bathroom), it might still be effective up to 12 months past expiration. But if it’s a liquid suspension, no-don’t take it. Even if it looks normal, it’s likely lost most of its strength. And never use expired antibiotics for serious infections like pneumonia or UTIs.
Do antibiotics become toxic after expiration?
There’s no strong evidence that most antibiotics turn toxic after expiration. The main risk is loss of potency, not poisoning. However, degraded tetracycline antibiotics can rarely cause kidney damage, but this is extremely rare with modern formulations. The bigger danger is treatment failure and antibiotic resistance.
How should I store antibiotics to make them last longer?
Keep them in their original container, away from heat, light, and moisture. A bedroom drawer or kitchen cabinet (away from the stove or sink) is ideal. Avoid bathrooms-they’re too humid. Use desiccants if available. Refrigeration helps for liquids, but never freeze unless instructed.
What should I do with expired antibiotics?
Don’t flush them or throw them in the trash. Take them to a pharmacy that offers a drug take-back program. Many pharmacies and hospitals collect expired meds for safe disposal. If that’s not available, mix them with coffee grounds or cat litter in a sealed container before tossing them-this reduces risk of accidental ingestion.
Are there any antibiotics that last longer than others after expiration?
Yes. Solid forms like doxycycline, cephalexin, and amoxicillin tablets tend to be more stable. Liquid forms like amoxicillin suspension, ceftriaxone, and penicillin injections degrade quickly. Beta-lactam antibiotics (penicillins, cephalosporins) are especially sensitive to moisture and heat, so they lose potency faster than others.
Can I use expired antibiotics if I’m in a remote area with no access to a pharmacy?
In true emergencies with no alternatives, some experts suggest using solid antibiotics up to 12 months past expiration if stored properly and visually intact. But only for mild infections-never for sepsis, meningitis, or serious wounds. This is a last-resort decision with serious risks. Seek medical help as soon as possible.
Rebecca Cosenza
November 19, 2025 AT 12:44Don't take expired antibiotics. Period. It's not worth the risk.
Even if it 'looks fine.' You're not a scientist. You're not a pharmacist. You're just guessing.
And guess what? Your guess could kill someone else.
swatantra kumar
November 19, 2025 AT 20:27Bro, I took amoxicillin from 2018 for a sinus infection last year.
Worked like a charm. 😎
Maybe the FDA is just scared of people saving money?
Also, my grandma used penicillin from the 60s. She lived to 97. Coincidence? I think not. 🤔
Cinkoon Marketing
November 20, 2025 AT 03:01Actually, there's a 2012 DoD study that found 90% of stockpiled antibiotics retained potency over 10+ years. The FDA's stance is more about liability than science. Most people don't realize that expiration dates are mostly marketing. Not science.
Also, storing meds in the bathroom? That's the real problem. Not the date on the bottle.
robert cardy solano
November 20, 2025 AT 22:12I used to work in a rural clinic. We had zero access to new meds for months at a time.
We used expired antibiotics all the time. Not for sepsis, obviously. But for UTIs? Ear infections? Yeah.
Most of the time it worked. Sometimes it didn't.
But we didn't have a choice.
And no, we didn't create superbugs. Not that I saw.
People are scared of what they don't understand.
Also, I've seen more harm from people hoarding antibiotics than from using expired ones.
Pawan Jamwal
November 22, 2025 AT 17:01India has been using expired meds for decades. And yet, we still have the lowest antibiotic resistance rates in the world? No? Wait... actually we have the highest.
So maybe the FDA is right after all. 🤷♂️
Also, your grandma's penicillin? That was pure. Now it's all synthetic garbage.
Modern pharma is a scam.
Bill Camp
November 23, 2025 AT 16:07THEY KNOW. THEY KNOW EXACTLY WHAT THEY'RE DOING.
Expiration dates are a scam to keep you buying new pills every year.
Big Pharma is laughing all the way to the bank while you're scared to use your $3 antibiotic.
They don't want you to be independent.
They want you dependent.
And now they're pushing 'AI potency testers' to make you pay even more.
Wake up, sheeple.
Lemmy Coco
November 25, 2025 AT 00:35my friend took some cephalexin that was 3 years out and it worked fine but i still dont reccomend it cause i dont want to be responcible for someone getting resistant superbugs
also i think the liquid ones are way more dangerous than pills
and yeah the bathroom thing is a joke
who stores meds in the bathroom? 😅
Nick Naylor
November 26, 2025 AT 23:16Let’s be clear: the FDA’s stance isn’t about fear-it’s about legal liability. Hospitals extend expiration dates because they have labs, quality control, and trained pharmacists. You? You have a drawer and a hunch. That’s not medicine. That’s Russian roulette with your microbiome.
And yes, the 2022 NIH data shows stability in tablets-but that’s under controlled humidity, not your 90% humidity bathroom. And even then, 85% potency isn’t 100%. You’re not treating a cold-you’re treating a bacterial infection that can kill you or create a superbug that kills your kid.
Stop romanticizing old pills. This isn’t survivalist fantasy. It’s public health. And your 'I got lucky' story? It’s contributing to a global crisis. You think you’re saving money? You’re paying for it in future ICU bills.
Also, the WHO estimates 4.3% of resistant infections are tied to expired meds. That’s 2.3 million people a year. Don’t be one of the reasons that number rises.
serge jane
November 28, 2025 AT 10:35There's something deeply human about wanting to trust what we already have
It's not just about antibiotics-it's about scarcity, about fear of waste, about believing that if something still looks the same, it still works the same
But biology doesn't care about our nostalgia
Our bodies don't remember what worked last time
And bacteria? They don't forget
Every time we take a weak dose, we're not just failing ourselves
We're training the enemy
And the enemy doesn't care if you're poor or desperate or just tired of being told what to do
The enemy just wants to survive
And it's winning
Maybe the real question isn't whether expired antibiotics work
But why we're so desperate to believe they do
Brianna Groleau
November 28, 2025 AT 16:45I grew up in a household where everything was reused-clothes, jars, food, even medicine.
My mom kept antibiotics in a Tupperware in the closet.
She used them for every sniffle.
She never went to the doctor.
She lived to 89.
But she also had five kidney infections, three ER trips, and a two-week hospital stay when she got sepsis from a UTI that didn't respond to her 'old amoxicillin.'
So yes, sometimes it works.
But when it doesn't? It breaks you.
And then you spend the next six months paying for it.
And the bacteria? They win.
And they’re still out there.
Waiting.
For your next kid.
Your next grandkid.
Your next excuse.
Don’t be the reason someone else pays the price.
Take it to the pharmacy.
It’s not expensive.
It’s not hard.
It’s just the right thing to do.
And if you can’t afford a new prescription?
Ask.
Someone will help.
They always do.
Just ask.
Rusty Thomas
November 30, 2025 AT 05:39OMG I JUST TOOK SOME EXPIRED CIPROFLOXACIN AND NOW I’M A SUPERHERO 🦸♀️
MY BACTERIA ARE SO SCARED THEY’RE QUITTING THEIR JOBS
THEY’RE STARTING A UNION AND DEMANDING BETTER WORK-LIFE BALANCE
AND NOW I HAVE TO PAY $1500 FOR A NEW PRESCRIPTION BECAUSE THEY’RE ALL ON STRIKE
AND THE FDA IS JUST WATCHING AND LAUGHING
WHY CAN’T WE JUST HAVE A NATIONAL ANTIBIOTIC RELIEF FUND
PLEASE SIGN MY PETITION
AND ALSO I’M SELLING MY OWN ‘EXPIRATION DATE TESTER’ APP
IT USES AI AND THERAPY
IT’S CALLED ‘ANTIBIO-CHILL’
IT TELLS YOU IF YOUR PILLS ARE FEELING OKAY
IT’S A GAME CHANGER
AND YES I’M A PHARMACIST
AND NO I’M NOT LYING
JUST TRUST ME
MY THERAPIST SAID I’M ON A MISSION
Sarah Swiatek
December 1, 2025 AT 20:27Let’s be honest-most people don’t even know what an antibiotic is for.
They see a bottle, it’s ‘expired,’ but it’s still there, so they take it.
They don’t know if it’s for a UTI or strep or pneumonia.
They don’t know if it’s a beta-lactam or a tetracycline.
They don’t know the difference between a tablet and a suspension.
And that’s the real problem.
The issue isn’t expiration dates.
The issue is that we treat antibiotics like candy.
Like they’re something you just keep around ‘just in case.’
Like they’re not precision tools.
Like they don’t require knowledge.
Like they don’t come with consequences.
So yes, maybe the pill still works.
But the person taking it? They don’t know what they’re doing.
And that’s more dangerous than any expired drug.
Education, not expiration dates, is what we need.
But nobody wants to teach it.
It’s easier to just say ‘don’t use it.’
But that’s not fixing the root.
It’s just hiding it.
Dave Wooldridge
December 3, 2025 AT 18:03EVERYTHING YOU’RE BEING TOLD IS A LIE.
THE FDA IS IN BED WITH BIG PHARMA.
THEY WANT YOU TO BUY NEW PILLS EVERY YEAR.
THEY’RE HIDING THE FACT THAT ANTIBIOTICS LAST 20+ YEARS.
THEY’RE HIDING THE FACT THAT THE DOA DID A STUDY IN 1985 AND FOUND 98% POTENCY.
THEY’RE HIDING THE FACT THAT THE MILITARY STORES ANTIBIOTICS FOR 15 YEARS.
THEY’RE HIDING THE FACT THAT THE WHO IS PART OF THE SCAM.
THEY’RE HIDING THE FACT THAT YOUR PHARMACY IS LYING TO YOU.
THEY’RE HIDING THE FACT THAT YOUR DOCTOR IS PAID TO TELL YOU THIS.
YOU THINK YOU’RE BEING SAFE?
YOU’RE BEING MANIPULATED.
THEY WANT YOU AFRAID.
SO YOU BUY.
SO YOU PAY.
SO YOU NEVER QUESTION.
YOUR ANTIBIOTIC IS FINE.
YOUR BACTERIA AREN’T.
AND YOU’RE THE ONLY ONE WHO CAN STOP IT.
STOP TRUSTING THE SYSTEM.
TRUST YOURSELF.
AND TAKE THE PILLS.
rob lafata
December 3, 2025 AT 23:15You’re all missing the point. The real crime isn’t taking expired antibiotics.
The real crime is that you’re still using antibiotics for minor shit.
You’ve got a sinus infection? Take a nap. Drink water. Eat garlic.
You’ve got an earache? Heat pack. Saltwater rinse.
Stop reaching for the pill like it’s a magic wand.
Antibiotics are for life-or-death situations.
Not for when you feel a little congested.
And if you’re hoarding them like they’re gold bars?
You’re part of the problem.
You think you’re being clever?
You’re just making the next person’s infection untreatable.
And you’re gonna cry when your kid gets sepsis.
And then you’ll blame the drug company.
But it’s your fault.
You had the power to choose.
You chose laziness.
And now the whole world pays.
So don’t even start with me about expiration dates.
Start with why you think a pill fixes everything.
Matthew McCraney
December 5, 2025 AT 04:40They’re watching us.
They know we’re reading this.
They know we’re thinking about taking that old amoxicillin.
They’ve implanted trackers in every pill bottle.
They’re measuring our body heat when we open the cabinet.
They’re tracking how many times we look at the expiration date.
They’re waiting for us to make the wrong choice.
So they can label us ‘high-risk’
and raise our insurance.
and deny us care.
and put us on a list.
They’re not worried about superbugs.
They’re worried about us getting too smart.
And they’ll do anything to keep us dependent.
Even lie about expiration dates.
Don’t trust the label.
Trust your gut.
And if you feel it… take it.
They can’t stop you.
Not really.
Nick Naylor
December 5, 2025 AT 12:07And that’s exactly why this post matters.
You think I’m being dramatic?
Look at the data: 98.7% resistance with expired antibiotics vs. 14.3% with fresh.
That’s not a fluke.
That’s evolution.
And it’s happening in real time.
Every time someone says ‘it worked for me,’ they’re not just risking their own health.
They’re handing bacteria a genetic upgrade.
And those upgrades? They spread.
Through family.
Through travel.
Through hospitals.
Through air.
Through water.
Through you.
So no.
It’s not ‘just me.’
It’s everyone.
And the next person who gets a UTI that doesn’t respond to any drug?
They might be your sister.
Your friend.
Your child.
Don’t be the reason they’re out of options.
Take it to the pharmacy.
It’s not a sacrifice.
It’s a responsibility.