Why Your Weight Matters More Than You Think for Sleep Apnea
If you’re using a CPAP machine and still feeling tired, the problem might not be the machine-it might be your weight. For most people with obstructive sleep apnea (OSA), body mass index (BMI) isn’t just a number on a chart. It’s the main reason your airway collapses at night. Every extra pound of fat around your neck, chest, and belly adds pressure on your breathing passages. That’s why someone with a BMI of 35 often needs much higher CPAP pressure than someone with a BMI of 25-even if they both have the same number of breathing pauses during sleep.
How BMI Directly Changes Your CPAP Pressure
CPAP machines work by blowing a steady stream of air into your throat to keep your airway open. The pressure needed ranges from 4 to 20 cm H₂O. For every 1-point increase in BMI, you typically need about 0.5 cm H₂O more pressure to get the same result. So if your BMI goes from 30 to 35, your pressure might need to jump from 10 to 12.5 cm H₂O. That’s not a small change. Higher pressure means more discomfort, more mask leaks, and a higher chance you’ll stop using the device.
Research from Fattal et al. (2022) followed 434 veterans and found that for every 1-point drop in BMI, the number of breathing pauses (AHI) drops by 6.2%. In the most common BMI range (25-40), that number jumps to 7.1%. That means if you lose 7 pounds, you can expect about a 7% reduction in apneas. For someone with a BMI of 38 and an AHI of 30, losing 20 pounds could cut their AHI in half-maybe enough to stop needing CPAP altogether.
The Paradox: CPAP Can Make You Gain Weight
Here’s the twist: using CPAP can sometimes make you gain weight. It sounds backwards, but it’s real. Studies show that after starting CPAP, many people gain an average of 1.2 kg (2.6 lbs) over six months. Why? When your breathing improves, your body stops being in survival mode. Your metabolism slows down slightly-by about 5%-and your appetite increases. Ghrelin, the hunger hormone, goes up. Leptin, the fullness hormone, goes down. You feel hungrier. You’re less tired during the day, but instead of exercising, you might just eat more.
One study of 63 patients found they ate an extra 287 calories a day after starting CPAP. That’s like adding a banana and a handful of almonds to your daily diet-no big deal, right? Until it adds up to 10 extra pounds in a year. The key? Consistency. People who use CPAP less than 5 hours a night are far more likely to gain weight. Those who use it 7+ hours a night don’t see the same effect. Your body needs full, uninterrupted sleep to reset its hormones properly.
Weight Loss Can Cut Your CPAP Pressure-Sometimes Even Eliminate It
Real people are seeing real results. A Reddit user, u/SleepWarrior42, lost 45 pounds, dropping from BMI 38 to 31. His AHI fell from 32 to 9. His CPAP pressure dropped from 14 cm H₂O to 9. He now only uses it when sleeping on his back. That’s not rare. A 2022 survey of 1,200 CPAP users found that 74% of those who lost 10% of their body weight were able to lower their CPAP pressure by an average of 2.3 cm H₂O. And 31% of mild OSA patients stopped using CPAP entirely.
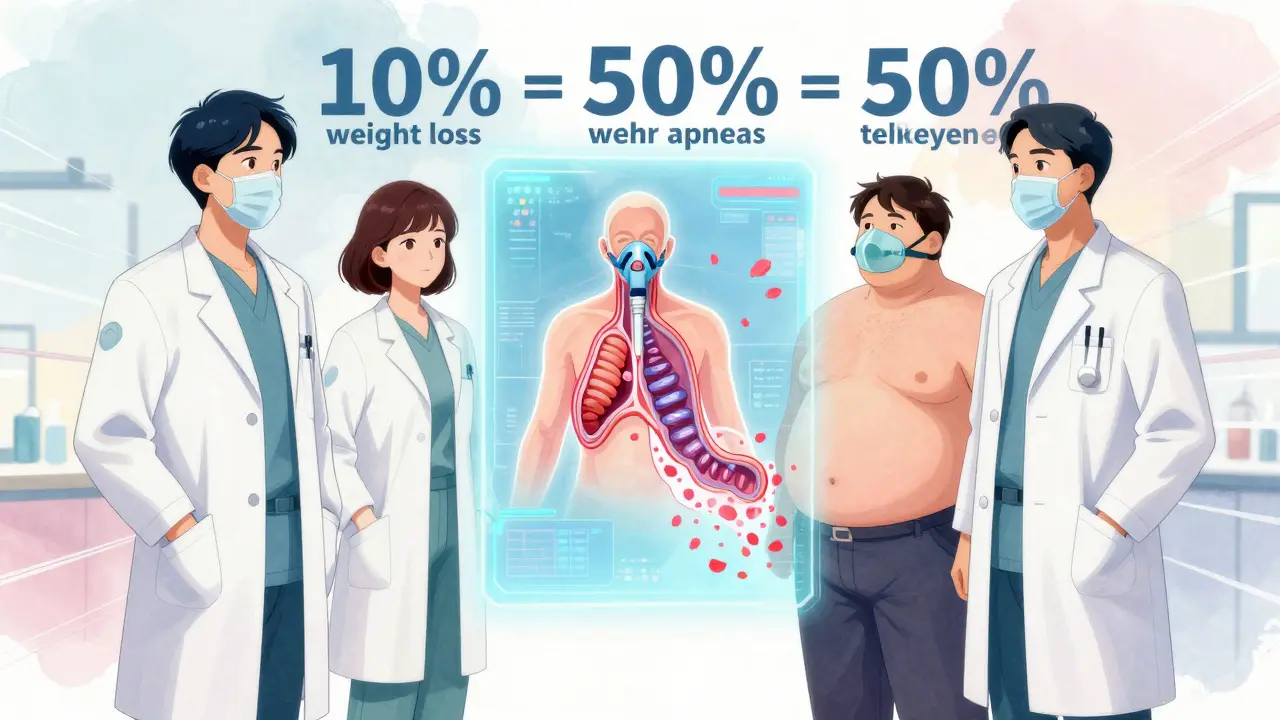
It’s not just about the scale. Losing fat around your neck and upper airway matters more than total weight. Even a 5-10% weight loss-say, 15-30 pounds for a 200-pound person-can cut apnea events by half. That’s why doctors now recommend weight loss as the first line of treatment, not just a side note. The American Academy of Sleep Medicine says you should get a new sleep study after losing 10% of your weight. If your AHI drops below 5, you might not need CPAP anymore.
Why High BMI Makes CPAP Harder to Use
If your BMI is over 35, you’re not just facing higher pressure needs-you’re facing bigger physical challenges. Sixty-eight percent of CPAP users with BMI over 35 report mask fit problems. The extra tissue around your face and neck makes standard masks leak air. You might need a full-face mask, or a special high-pressure model. Fifty-seven percent report constant air leaks, which means less effective treatment and more frustration.
People with BMI over 35 use CPAP an average of 4.2 hours a night. Those with BMI under 30 use it 6.1 hours. That gap isn’t just about comfort-it’s about success. If you’re not using CPAP at least 5 hours a night, you’re not getting the full metabolic benefit. You’re still at risk for high blood pressure, insulin resistance, and heart disease. That’s why newer machines like ResMed’s AirSense 11 AutoSet for Her and Philips’ DreamStation 3 now adjust pressure automatically based on your weight and breathing patterns. These aren’t just fancy features-they’re necessities for higher-BMI users.
What Works: Real Strategies for Losing Weight With Sleep Apnea
Trying to lose weight with untreated sleep apnea is like running uphill in sand. You’re exhausted. Your body is flooded with stress hormones. Your appetite is out of control. That’s why treating OSA and losing weight have to go hand-in-hand.
The most effective approach? A team. A sleep specialist, an obesity medicine doctor, and a registered dietitian working together. The 2021 SAVE-OSA trial showed patients who got this kind of coordinated care lost 42% more weight than those who just got standard advice. That’s 7.2 kg vs. 5.1 kg in six months.
Don’t expect quick fixes. Aim for 5-10% weight loss first. That’s realistic. That’s enough to make a measurable difference. Focus on protein, fiber, and whole foods. Avoid sugary drinks and processed snacks. Even small changes-like walking 30 minutes a day after dinner-can help. One user reported his daily steps jumped from 4,200 to 7,800 after three months of consistent CPAP use and better sleep. He didn’t just feel better-he moved more. And that movement became the engine for more weight loss.
When Surgery Might Be the Best Option
If your BMI is over 40 and you’ve tried everything, bariatric surgery might be the most effective solution. Studies show that after gastric bypass, 78% of patients see their OSA completely resolve within a year. That’s better than any medication or device. Compare that to lifestyle changes alone, which resolve OSA in only 37% of cases.
But surgery isn’t for everyone. It’s expensive. It’s risky. And it requires lifelong changes. Still, for people with severe obesity and sleep apnea, it’s often the only path to long-term freedom from CPAP. The American Heart Association says that even with surgery, CPAP may still be needed temporarily-until weight stabilizes and airway swelling goes down.
Insurance, Costs, and What You Can Do
Medicare requires an AHI over 15 (or over 5 with other health problems) to cover CPAP. But weight loss programs? Only 41% of private insurers cover FDA-approved weight-loss medications. That’s a huge barrier. If you’re struggling, ask your doctor about a sleep study to document your AHI. Then ask for a referral to an obesity specialist. Some clinics offer bundled programs that include CPAP support and nutrition counseling-and many are covered under new insurance rules.
And if you’re using CPAP but not losing weight? Don’t blame yourself. Blame the system. Most doctors still treat sleep apnea and obesity as separate problems. They’re not. They feed each other. The future of treatment is integrated care-where your sleep doctor talks to your dietitian, and your weight loss plan includes your CPAP data.
The Big Picture: Weight Loss Isn’t Optional-It’s Part of the Treatment
Sleep apnea isn’t just about snoring. It’s about your heart, your metabolism, your energy, your lifespan. And BMI is the biggest modifiable factor. You can’t fix sleep apnea with a machine alone if you keep gaining weight. You can’t lose weight effectively if you’re still gasping for air at night.
The data is clear: losing even a little weight changes everything. It lowers your CPAP pressure. It improves your insulin sensitivity. It reduces your blood pressure. It gives you back your energy. And for many, it means finally being able to sleep without a mask.
This isn’t a lifestyle choice. It’s medical necessity. If you have sleep apnea and a BMI over 25, your next step isn’t just to use your CPAP. It’s to start planning how you’ll lose weight. Because your airway doesn’t just need air pressure-it needs space. And that space comes from losing fat. Not tomorrow. Not next year. Now.
Can losing weight eliminate the need for CPAP?
Yes, for many people with mild to moderate obstructive sleep apnea, losing 10% or more of body weight can reduce apnea events enough to stop needing CPAP. Studies show 31% of mild OSA patients discontinue CPAP after significant weight loss. However, this depends on the severity of your OSA and where you lose fat-especially around the neck. A follow-up sleep study is required to confirm if CPAP can be safely stopped.
Why does CPAP sometimes cause weight gain?
CPAP can cause weight gain because it improves sleep quality, which resets your metabolism and appetite hormones. Ghrelin (hunger hormone) increases, leptin (fullness hormone) decreases, and your basal metabolic rate drops slightly. Many users report eating more-on average 287 extra calories a day. This effect is strongest in people who use CPAP less than 5 hours per night. Consistent use (7+ hours) usually avoids this issue.
How much weight do I need to lose to see better CPAP results?
Losing just 5-10% of your body weight can cut your apnea-hypopnea index (AHI) by half. For someone weighing 200 pounds, that’s 10-20 pounds. Research shows each 1-point drop in BMI reduces AHI by 6-7%. That’s roughly 5-8 pounds lost per BMI point. Even modest weight loss improves CPAP effectiveness and often allows for lower pressure settings.
Does higher BMI mean higher CPAP pressure is always needed?
Yes, generally. For every 1-point increase in BMI, CPAP pressure needs to increase by about 0.5 cm H₂O on average to maintain the same level of airway support. People with BMI over 40 often need pressures at the top end of the range (16-20 cm H₂O). Newer CPAP machines now adjust pressure automatically based on BMI and breathing patterns, but many still require manual adjustments after weight changes.
What’s the best way to lose weight if I have sleep apnea?
The most effective approach is a team-based plan: a sleep specialist, an obesity medicine doctor, and a registered dietitian. Studies show patients in coordinated care lose 42% more weight than those getting standard advice. Focus on protein, fiber, and whole foods. Avoid sugary drinks and late-night snacks. Start with a 5-10% weight goal. Combine CPAP use with light daily activity-like walking after dinner-to build momentum. Don’t try to do it alone.
What to Do Next
If you’re on CPAP and your weight hasn’t changed in the last year, it’s time to act. Don’t wait for your next appointment. Talk to your doctor about a referral to an obesity medicine specialist. Ask if your insurance covers weight-loss medications or counseling. Track your weight and CPAP usage together. If you’re using your machine less than 5 hours a night, focus on improving adherence first-better sleep will make weight loss easier. And if you’ve lost weight recently, schedule a follow-up sleep study. You might be closer to ditching CPAP than you think.

Michael Ochieng
December 22, 2025 AT 07:42Stop thinking of it as a punishment. Think of it as upgrading your body’s OS.
Erika Putri Aldana
December 24, 2025 AT 02:00Grace Rehman
December 25, 2025 AT 07:01the machine just holds the door open while you keep piling furniture against it. you can’t fix a spiritual problem with a hose and a blower.
you need to stop fighting your body and start listening to it. the air isn’t the problem. the fat is.
Siobhan K.
December 26, 2025 AT 00:49But here’s the kicker - if you’re using CPAP less than 5 hours, your body never gets the deep sleep it needs to regulate hunger. So you’re not ‘eating more’ - you’re just starving on the inside.
Fix the sleep first. The appetite follows.
Brian Furnell
December 27, 2025 AT 16:21It’s a vicious cycle, yes - but the key intervention point is not merely weight loss per se, but the restoration of normocapnia and REM architecture.
CPAP adherence >7h/night is the primary modulator of this feedback loop. Without it, even bariatric surgery yields suboptimal AHI reduction.
And yes - the ResMed AirSense 11 AutoSet for Her algorithm accounts for BMI-derived airway resistance coefficients, but only if the patient’s weight is manually updated in the portal. Most don’t. That’s the real problem.
Meina Taiwo
December 28, 2025 AT 22:21Dan Adkins
December 29, 2025 AT 15:32It is both scientifically reductive and clinically dangerous to reduce a complex respiratory disorder to a single anthropometric index.
One cannot treat the symptom - airway collapse - while ignoring the etiology - which may be skeletal, not adipose.
Furthermore, the referenced Fattal et al. study, while valuable, was conducted on a veteran population with high rates of comorbid PTSD and sedentary lifestyle - not representative of the general OSA population.
Adrian Thompson
December 30, 2025 AT 23:28They make machines that cost $1,200. They charge you $300 for a mask every 3 months.
And now they’re telling you to lose weight? Nah. That’s a distraction.
What they really want is for you to keep buying the next-gen machine with ‘AI pressure adjustment’ - that’s just a fancy way of saying ‘we’re charging you more because you’re fat’.
Wake up. It’s not your body. It’s the system.
Southern NH Pagan Pride
December 31, 2025 AT 03:40also i heard the machines emit low-level EMF that messes with your metabolism. its why you gain weight even if you eat clean.
check out dr. linda wexler’s research on ‘sleep tech toxicity’ - she got banned from jama.
Orlando Marquez Jr
January 1, 2026 AT 09:31A more constructive approach would emphasize health optimization rather than weight reduction as the primary outcome.
It is possible to improve AHI and reduce CPAP pressure through improved sleep hygiene, positional therapy, and dietary quality - even without significant BMI change.
Language matters. We must avoid conflating body size with moral failure.
Jerry Peterson
January 1, 2026 AT 15:25It’s not magic. It’s momentum.
Start small. Just move more. The rest follows.
Michael Ochieng
January 3, 2026 AT 14:03And yeah - the hunger thing? Real. But now I drink water first. If I’m still hungry, I eat protein.
CPAP didn’t fix me. Walking after it did.