What Is Thyroid Eye Disease?
Thyroid Eye Disease (TED) isn’t just about your thyroid. It’s an autoimmune condition where your body’s immune system attacks the tissues behind your eyes-muscles, fat, and connective tissue. This causes swelling, inflammation, and pressure that pushes your eyeballs forward. You might not even have an overactive thyroid when it starts. About half of people with Graves’ disease get TED, but it can also show up in people with normal or low thyroid levels. It’s not rare: roughly 16 out of every 100,000 people develop it each year. Women are four to six times more likely to get it than men, and it most often hits people between 40 and 60.
What Are the Symptoms?
People with TED don’t just have watery eyes. The symptoms are specific and often get worse over time. A gritty, sandy feeling in the eyes? That’s common-reported by 78% of patients. Light sensitivity? Around 65%. Pain when you move your eyes? That’s 52%. Redness from swollen conjunctiva, dry eyes, excessive tearing, puffy eyelids-all show up frequently. The most visible sign is bulging eyes, called proptosis, which affects about 31% severely. Double vision happens in nearly 1 in 4 cases. And it’s usually both eyes: 89% of cases are bilateral. If you notice these symptoms together, especially if you have a history of thyroid problems, don’t wait. Early signs matter.
Why Does It Happen?
The root cause is antibodies that target the TSH receptor. These same antibodies that cause Graves’ disease also bind to cells behind the eyes. That triggers inflammation and fat buildup. Smoking is the biggest risk factor-people who smoke are nearly eight times more likely to develop TED. High levels of TRAb antibodies (above 15 IU/L) also raise your risk. Even more surprising: radioactive iodine treatment for Graves’ can make TED worse if you don’t get steroids at the same time. That’s why doctors now check your TRAb levels early and often. If they’re high, they’ll plan ahead to protect your eyes.
How Is It Staged?
Doctors don’t treat all TED the same. They use the Clinical Activity Score (CAS), a checklist of symptoms like redness, swelling, and pain. A score of 3 or higher means active disease-your eyes are still inflaming, and you need treatment fast. Mild TED (CAS under 3) might just need lubricating eye drops. Moderate-to-severe TED (CAS 3 or higher) needs stronger medicine. Sight-threatening TED is the worst: vision loss from pressure on the optic nerve or corneal damage. That’s an emergency. Imaging like CT or MRI shows which eye muscles are swollen-usually the bottom one (85%), then the inner one (75%). This helps predict how bad things might get.
Steroids: The Traditional Treatment
For years, steroids have been the go-to for active TED. The most effective form is intravenous methylprednisolone. You get 500 mg once a week for six weeks, then 250 mg weekly for another six. About 60 to 70% of people see real improvement-less swelling, less double vision, less pain. Oral prednisone is cheaper and easier, but it’s less effective and causes more side effects: weight gain (on average 8.2 kg), high blood sugar, bone loss. The European guidelines say don’t go over 4.5 to 5 grams total IV dose-it can hurt your liver. Even then, about a quarter of people relapse after stopping steroids. That’s why many now turn to newer options.
Biologics: A Game-Changer
Enter teprotumumab (Tepezza®). Approved by the FDA in 2020, it’s the first treatment that targets the actual cause of TED-not just suppressing inflammation, but blocking the IGF-1 receptor that drives the disease. In the OPTIC trial, 71% of patients saw their eyes bulge back by at least 2 millimeters. Only 20% did in the placebo group. Double vision improved in 59% of those on teprotumumab versus 26% on placebo. The treatment is eight infusions over 21 weeks. But it’s expensive: around $360,000 in the U.S. Insurance often denies it, and the prior authorization process can take over six weeks. Still, patient satisfaction is higher than with steroids-74% vs. 58%. Side effects include muscle cramps, hearing changes, and high blood sugar. But for many, the trade-off is worth it.
Other Biologics and What’s Coming
Teprotumumab isn’t the only option on the horizon. Satralizumab (Enspryng®), an anti-IL-6 drug, got FDA approval in 2023 and is given as a monthly shot. Early data shows about half of patients respond. Rituximab and tocilizumab are being tested too, but evidence is still weak. The biggest news? A biosimilar to teprotumumab is coming by 2025 and could cut costs by 30 to 40%. There’s also a trial combining teprotumumab with selenium-early results show an 82% response rate, better than either alone. Researchers are now looking for genetic markers that predict who’ll respond best. In five years, we might be able to test your DNA and know exactly which treatment to start.
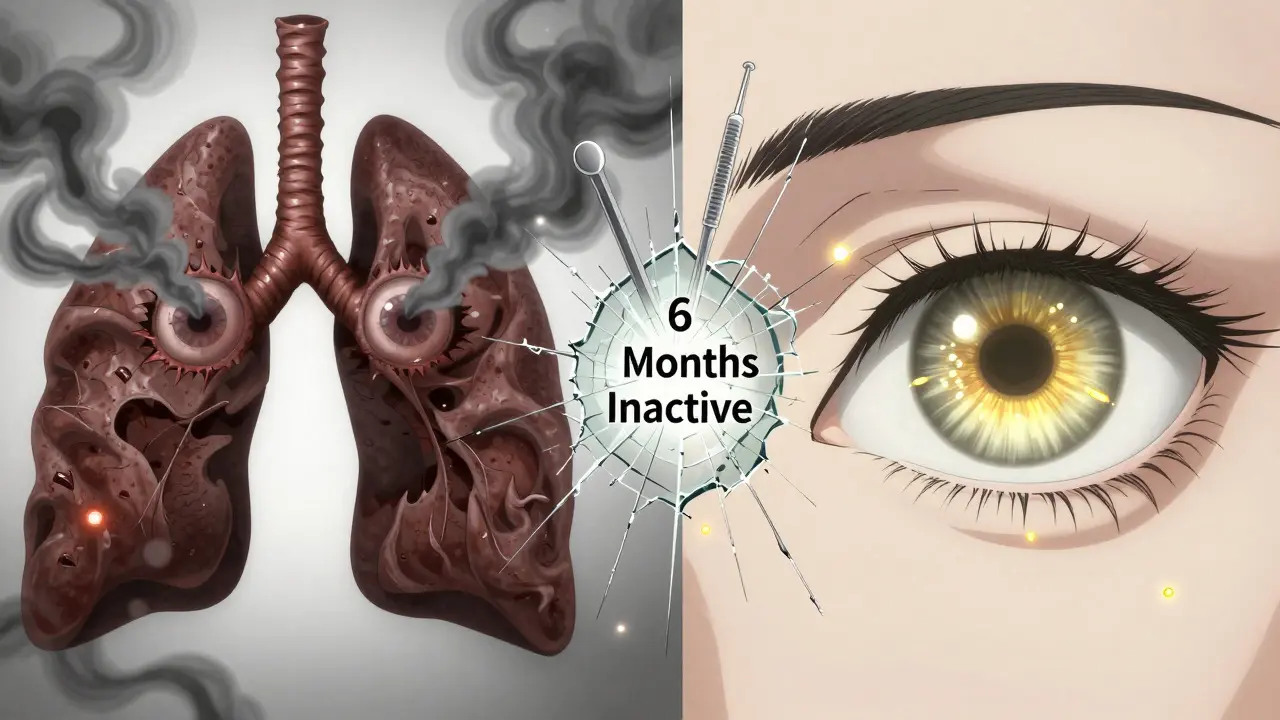
What About Surgery?
Surgery isn’t the first step-it’s the last. Orbital decompression, which removes bone to give your eye more room, can reduce bulging by 2 to 5 millimeters. But it carries risks: 15% of people get new or worse double vision, 8% get sinus infections, and 0.5% risk vision loss. Strabismus surgery fixes eye alignment after inflammation settles. Eyelid surgery corrects retraction. All of these are done only after the disease has been inactive for at least six months. No one wants to operate on active inflammation-it makes things worse.
Practical Management Tips
For mild TED: use preservative-free artificial tears (0.15-0.3% sodium hyaluronate). Most people feel better in four weeks. Selenium supplements (200 mcg daily) help a little-Cochrane found a small but real boost in quality of life. For moderate-to-severe: start IV steroids within two weeks of symptoms. Delay past eight weeks and your chances of success drop from 65% to 42%. Prisms in glasses help with double vision, but only if the muscle misalignment is under 15 prism diopters. Beyond that, surgery is needed. Quitting smoking is non-negotiable. It’s the single most powerful thing you can do to stop TED from getting worse.
Access and Cost Challenges
Even though biologics work better, many patients can’t get them. In the U.S., 42% of patients face insurance denials for teprotumumab. Medicaid patients are hit hardest-67% struggle with access compared to 28% of those with private insurance. One Reddit user said each infusion cost $5,000 out-of-pocket, even with insurance. The drugmaker, Amgen (which bought Horizon Therapeutics), has patient assistance programs, but navigating them takes time and persistence. In rural areas, only 28% of ophthalmologists have access to TED specialists. If you’re in a small town, you may need to travel for proper care.
What’s Next?
Thyroid Eye Disease is no longer just a side effect of thyroid problems. It’s a standalone condition with targeted treatments. The market for TED drugs is growing fast-projected to hit $4.7 billion by 2030. But progress isn’t just about new drugs. It’s about catching it early, treating it right, and making sure everyone has access. The future holds personalized medicine: genetic tests to predict risk, biomarkers to match you with the best drug, and cheaper biosimilars to make treatment fairer. Right now, if you have TED, your best move is to see a specialist-endocrinologist and ophthalmologist together-as soon as symptoms appear. Don’t wait for the eyes to bulge. Don’t wait for double vision to start. Act early. Your vision depends on it.

beth cordell
January 11, 2026 AT 17:05Sonal Guha
January 13, 2026 AT 15:16laura manning
January 14, 2026 AT 03:42Faith Wright
January 15, 2026 AT 01:48Rebekah Cobbson
January 16, 2026 AT 05:55Craig Wright
January 17, 2026 AT 05:10Audu ikhlas
January 19, 2026 AT 03:04Jay Powers
January 20, 2026 AT 23:36Lelia Battle
January 21, 2026 AT 02:07Sumit Sharma
January 22, 2026 AT 21:15George Bridges
January 23, 2026 AT 13:05