SSRI-NSAID GI Bleeding Risk Calculator
Assess Your Risk
Your Risk Assessment
Combined risk multiplier:
Combining SSRIs and NSAIDs might seem harmless - one for your mood, the other for your aches. But together, they can quietly raise your risk of a dangerous GI bleeding event. This isn’t theoretical. It’s happening in real patients, often without warning.
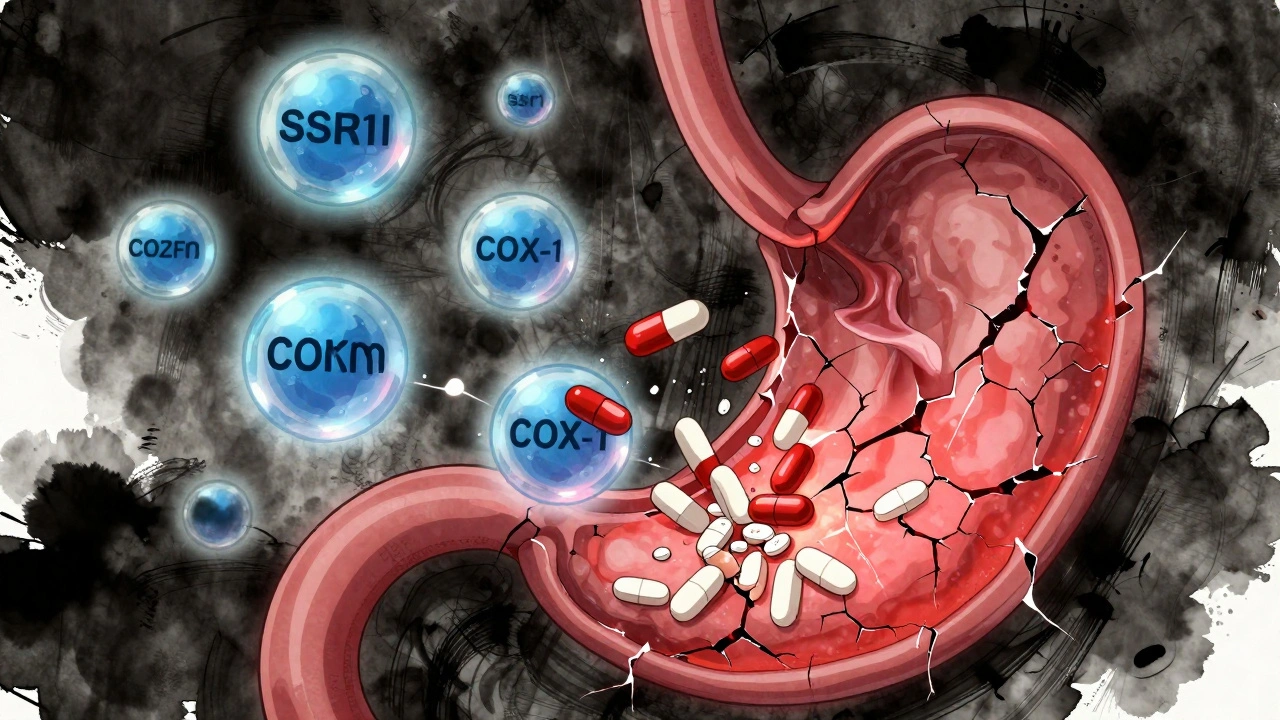
Why This Combination Is Riskier Than You Think
SSRIs like sertraline, fluoxetine, and citalopram work by increasing serotonin in the brain to help with depression and anxiety. But serotonin also plays a key role in blood clotting. Platelets need serotonin to stick together and seal off damaged blood vessels. When SSRIs block serotonin reuptake into platelets, those platelets become less effective at forming clots. That means even a small tear in your stomach lining - something that would normally heal quickly - can start bleeding and keep bleeding. NSAIDs like ibuprofen, naproxen, and diclofenac cause their own damage. They shut down COX-1 enzymes, which are responsible for making protective prostaglandins in your stomach lining. Without those prostaglandins, your stomach loses its natural shield: less mucus, less blood flow, slower healing. So you get tiny erosions. And when those erosions meet SSRIs’ weakened clotting ability? The risk skyrockets. Studies show that taking just an SSRI raises your GI bleeding risk by about 40-50%. Taking just an NSAID? That risk jumps 2 to 4 times, depending on the drug. But together? The risk doesn’t just add up - it multiplies. A 2023 meta-analysis confirmed a 75% increase in upper GI bleeding risk when both are taken together. That’s not a small bump. That’s a major red flag.Who’s Most at Risk?
Not everyone who takes both drugs will bleed. But some people are sitting on a ticking clock.- People over 65: Aging stomachs heal slower. Blood vessels become more fragile. The risk spikes dramatically after age 65.
- Those with a history of ulcers or GI bleeding: If you’ve had a bleed before, your stomach lining is already damaged. Adding SSRIs and NSAIDs is like pouring salt on an open wound.
- People on blood thinners: Warfarin, apixaban, or even low-dose aspirin? Add SSRIs and NSAIDs to the mix, and you’re stacking three bleeding risks on top of each other.
- Those taking high-dose or long-term NSAIDs: Daily use of naproxen or diclofenac for arthritis? That’s a major contributor to mucosal damage.
Even if you’re young and healthy, don’t assume you’re safe. Many people don’t know they have a silent H. pylori infection - a common bacteria that causes stomach ulcers. If you’re on SSRIs and NSAIDs and have H. pylori, your bleeding risk is even higher.
Which Drugs Are the Worst?
Not all SSRIs or NSAIDs are created equal when it comes to bleeding risk.NSAIDs:
- Highest risk: Naproxen, diclofenac, piroxicam - these strongly inhibit COX-1 and cause the most mucosal damage.
- Moderate risk: Ibuprofen - still risky, but slightly less damaging than others. Still dangerous when paired with SSRIs.
- Lowest risk: Celecoxib - a COX-2 selective NSAID. It doesn’t hurt your stomach lining as much. Studies show its bleeding risk is close to baseline - especially when compared to naproxen or diclofenac.
SSRIs:
- All SSRIs carry similar bleeding risk because they work the same way - blocking serotonin reuptake in platelets.
- Some studies suggest escitalopram may be slightly less risky than fluvoxamine or paroxetine, but the difference is small and not enough to rely on.
- Don’t assume one SSRI is “safe” because it’s newer or more popular.
Bottom line: If you’re on an SSRI and need pain relief, avoid naproxen and diclofenac. Ibuprofen is the least bad NSAID option - but still risky. Celecoxib is the safest NSAID choice if you can use it.

What You Can Do: Prevention That Works
The good news? This risk is preventable. You don’t have to choose between managing pain and managing depression.Step 1: Ask if you really need both.
- Can your pain be managed with acetaminophen (paracetamol)? It doesn’t affect platelets or stomach lining. For many people, it’s enough.
- Is there an alternative to SSRIs? Bupropion (Wellbutrin) doesn’t interfere with platelets. If your depression allows it, switching might eliminate the bleeding risk entirely.
Step 2: If you must take both, use a PPI.
Proton pump inhibitors - like omeprazole, esomeprazole, or pantoprazole - are the gold standard for protection. They reduce stomach acid enough to let your lining heal and reduce the chance of ulcers forming. Studies show that adding a daily PPI cuts the excess bleeding risk from SSRI-NSAID use by about 70%. That brings the risk back down to near-normal levels.
Take 20mg of omeprazole daily. Don’t wait until you feel symptoms. Prevention is the only reliable strategy.
Step 3: Get tested for H. pylori.
If you’re on long-term NSAIDs and SSRIs, ask your doctor for a simple breath or stool test for H. pylori. If it’s positive, eradicating the infection can cut your bleeding risk in half. The American College of Gastroenterology now recommends testing before starting dual therapy for high-risk patients.
What Doctors Are (and Aren’t) Doing
Here’s the uncomfortable truth: many doctors don’t know or don’t talk about this risk.A 2021 survey of 1,200 primary care doctors found that only 39% routinely check for this interaction. Just 22% prescribe PPIs as a preventive step. That means most patients are being prescribed this dangerous combo without any protection.
Patients aren’t being warned either. In a 2022 survey, 68% of people taking both drugs said they were never told about the bleeding risk. That’s not negligence - it’s systemic oversight. The interaction isn’t flashy. It doesn’t cause immediate side effects. So it gets missed.
But hospitals are catching on. Cleveland Clinic added automated alerts to their electronic records in 2019. After that, upper GI bleeding admissions dropped by 42% among patients on both drugs. Mayo Clinic and others followed. Technology can help - but only if doctors listen to it.
Real Stories, Real Consequences
Online forums are full of people who didn’t know the danger until it was too late.One Reddit user described black, tarry stools for three days before ending up in the ER. Another said they’d been taking sertraline and ibuprofen for years - no issues, until one morning they passed out from blood loss. Both had no prior history of ulcers. Neither had been warned.
On the other side, there are success stories. A user on Drugs.com with rheumatoid arthritis and depression switched from naproxen to celecoxib, added omeprazole, and stayed symptom-free for 18 months. That’s the blueprint.
What’s Next: New Tools and Guidelines
The science is evolving fast.In 2023, researchers introduced a new risk-prediction model that factors in your genes - specifically CYP2C19 mutations. These affect how you metabolize both SSRIs and PPIs. If you’re a slow metabolizer, PPIs might not work as well. That could mean you need a higher dose or a different one.
Pharmaceutical companies are testing new NSAID formulations with built-in PPIs. One dual-release capsule - ibuprofen plus omeprazole - is in Phase III trials. If approved, it could make safe pain relief easier for people who need both drugs.
And AI is stepping in. A 2023 study used machine learning to analyze electronic health records and predict individual bleeding risk with 86% accuracy. Imagine a system that flags your risk before you even get the prescription.
By 2024, the American College of Gastroenterology is expected to update its guidelines to make PPI co-therapy standard for anyone on long-term SSRI-NSAID combinations - especially if they’re over 65 or have any other risk factor.
Your Action Plan
If you’re taking an SSRI and an NSAID right now:- Don’t stop either drug on your own. Talk to your doctor first.
- Ask: “Is there a safer painkiller I can use instead of this NSAID?”
- If you must keep both: Ask for a proton pump inhibitor like omeprazole 20mg daily.
- Ask for an H. pylori test. It’s simple, non-invasive, and changes your risk profile.
- Watch for warning signs: Black or tarry stools, vomiting blood, dizziness, or sudden abdominal pain. Go to the ER if any appear.
This isn’t about fear. It’s about awareness. You’re not alone in taking these drugs. But you deserve to know the real risks - and how to stay safe.
Can I take ibuprofen with an SSRI?
Yes, but with caution. Ibuprofen is the lowest-risk NSAID, but combining it with an SSRI still increases your GI bleeding risk by about 75%. If you must use it, take it with a proton pump inhibitor like omeprazole and only for the shortest time possible. Avoid daily use unless absolutely necessary.
Is celecoxib safer than other NSAIDs when taking SSRIs?
Yes. Celecoxib is a COX-2 selective NSAID and doesn’t interfere with stomach-protecting prostaglandins the way traditional NSAIDs do. Studies show its GI bleeding risk is close to normal - especially compared to naproxen or diclofenac. If you need long-term pain relief and are on an SSRI, celecoxib is the preferred NSAID option.
Do all SSRIs increase bleeding risk equally?
Most SSRIs carry similar risk because they all inhibit serotonin reuptake in platelets. Fluoxetine, sertraline, citalopram, escitalopram - they all affect clotting. Some studies suggest escitalopram may be slightly less risky, but the difference is too small to rely on. Don’t switch SSRIs hoping to reduce bleeding risk - focus on protecting your stomach instead.
Can I skip the PPI if I only take NSAIDs occasionally?
Even occasional NSAID use with an SSRI can be dangerous. There’s no safe threshold. A single dose can trigger bleeding in someone with a vulnerable stomach lining. If you’re on an SSRI, treat every NSAID dose - even one-time use - as a potential risk. Use acetaminophen instead, or use a PPI if you must take the NSAID.
How do I know if I’m having a GI bleed?
Signs include black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness, fainting, or sharp abdominal pain. These are medical emergencies. Don’t wait to see if it gets better. Call 999 or go to the ER immediately.
Should I get tested for H. pylori if I’m on SSRIs and NSAIDs?
Yes, especially if you’re over 60, have a history of ulcers, or are on long-term therapy. H. pylori infection doubles your risk of bleeding when combined with these drugs. A simple breath or stool test can detect it. If positive, treatment with antibiotics clears the infection and significantly lowers your risk.
Is there a safer antidepressant than SSRIs if I need NSAIDs?
Yes. Bupropion (Wellbutrin) doesn’t affect platelet serotonin and doesn’t increase bleeding risk. If your depression allows it, switching to bupropion can eliminate the interaction entirely. Talk to your doctor about whether it’s appropriate for your symptoms. Other options like mirtazapine or vortioxetine also have lower bleeding risk than SSRIs.
Don’t assume your doctor knows this risk. Don’t assume your meds are safe just because they’re commonly prescribed. Your stomach doesn’t have a voice - but you do. Ask the right questions. Push for protection. You’re not being paranoid. You’re being smart.
vinoth kumar
December 2, 2025 AT 16:59Wow, this is exactly why I switched from ibuprofen to acetaminophen after my doctor mentioned the SSRI interaction. I’m on sertraline for anxiety and didn’t realize how dangerous daily NSAIDs could be. PPIs are now non-negotiable for me. Thanks for laying this out so clearly.
shalini vaishnav
December 3, 2025 AT 18:27Typical Western medical overreaction. In India, we’ve been taking paracetamol and antidepressants together for decades without this panic. Your system overdiagnoses everything. The real issue is pharmaceutical marketing, not the drugs themselves.
bobby chandra
December 4, 2025 AT 19:26Let me be crystal clear: this isn’t just a ‘risk’-it’s a ticking time bomb in plain sight. The fact that 68% of patients aren’t warned? That’s not incompetence. That’s systemic negligence dressed up as ‘standard practice.’ If your doctor doesn’t bring up PPIs when prescribing SSRIs + NSAIDs, find a new doctor. Period.
Archie singh
December 5, 2025 AT 15:14They’re lying about celecoxib. It’s just a placebo with a fancy name. The real agenda? Pushing expensive brand-name drugs while burying the truth about how NSAIDs are designed to make you dependent. The FDA’s been compromised since 2004. You think they care about your stomach? They care about profit margins.
Gene Linetsky
December 7, 2025 AT 08:59Ever wonder why all the ‘safe’ alternatives like bupropion are harder to get? Because Big Pharma doesn’t make as much off them. They want you hooked on SSRIs and NSAIDs so you keep coming back for PPIs, endoscopies, and hospital visits. It’s a cash cow. Don’t be fooled.
Ignacio Pacheco
December 7, 2025 AT 22:42So… if I take a single ibuprofen for a headache while on escitalopram, am I basically signing a waiver for internal bleeding? Because that’s how it sounds. No wonder my uncle ended up in ICU last year. Nobody told him.
Jim Schultz
December 9, 2025 AT 19:34Let’s be honest-this is why I stopped trusting doctors. They prescribe SSRIs like candy, then hand you a naproxen script for your back pain, and never mention the bleeding risk. It’s not negligence-it’s arrogance. They assume you’ll ‘figure it out’ on Reddit. Well, here I am. And now you know.
Kidar Saleh
December 11, 2025 AT 07:41I’m a GP in London, and I can confirm-this interaction is grossly under-discussed. I now have a printed checklist for every patient on SSRIs: ‘NSAID use? PPI? H. pylori history?’ We’ve cut our GI bleed referrals by nearly half since implementing this. Knowledge is power-but only if it’s shared.
Chloe Madison
December 12, 2025 AT 01:40If you’re on an SSRI and you’re taking NSAIDs for more than 3 days a week-you need a PPI. Full stop. No exceptions. I’m not being dramatic. I’ve seen the charts. The risk isn’t theoretical. It’s measurable. It’s preventable. And yet, so many people are flying blind. Please, for your own sake-ask your doctor about omeprazole.
Makenzie Keely
December 13, 2025 AT 02:25Can we talk about how absurd it is that we have to be medical detectives just to avoid bleeding out? We’re told to take these drugs for chronic conditions, but the warnings are buried in 50-page PDFs no one reads. The system is broken. Someone needs to make a simple, one-page handout for every pharmacy. This shouldn’t be rocket science.
James Kerr
December 14, 2025 AT 05:57My grandma took ibuprofen and Zoloft for 8 years and never had an issue. Maybe it’s just not a big deal for everyone? I mean, I’ve seen people panic over coffee being ‘toxic’ too. Not everything needs to be a crisis.
Charles Moore
December 15, 2025 AT 18:49Thanks for this. I’ve been on fluoxetine and naproxen for years and never knew. I’m getting tested for H. pylori tomorrow and asking for omeprazole. Small steps, but this might save my gut. You’re right-we have to ask. We can’t wait for them to tell us.
Kara Bysterbusch
December 16, 2025 AT 10:05The real tragedy? This isn’t even the tip of the iceberg. What about SSRIs + anticoagulants? Or SSRIs + corticosteroids? Or SSRIs + NSAIDs + aspirin? The interaction web is a spider’s nightmare. We need mandatory clinical decision support built into every EHR-not just Cleveland Clinic’s version. This should be universal.
Rashmin Patel
December 16, 2025 AT 20:52OMG I’m so glad I found this!! I’ve been on sertraline and diclofenac for my arthritis and never thought twice!! I just had black stools last week but thought it was my diet!! I’m going to the doctor tomorrow to get tested for H. pylori and get a PPI!! I’m so scared but also so relieved I’m not alone!! 🙏❤️
sagar bhute
December 17, 2025 AT 06:13Everyone’s acting like this is some groundbreaking revelation. Newsflash: this has been in the British Medical Journal since 2017. The only reason it’s trending now is because influencers started posting about it. The science is old. The panic is new. And the real losers? The patients who got ignored for years.