Imagine ordering your favorite shrimp stir-fry at a busy Asian restaurant, only to break out in hives minutes later. Or worse - your throat starts closing, and you realize you didn’t bring your epinephrine. This isn’t rare. About 2% of people worldwide have a shellfish allergy, and for many, it’s the most dangerous food allergy they’ll ever face. Unlike peanut or egg allergies, shellfish allergy doesn’t always show up in childhood. In fact, it’s most common in adults over 40, and it often comes out of nowhere. What makes it even trickier is that you might be allergic to shrimp but safely eat scallops - or you might react to both. And here’s the twist: you could test positive for shellfish allergy without ever eating it, just because you’re allergic to dust mites.
Why Shellfish Allergy Is So Unpredictable
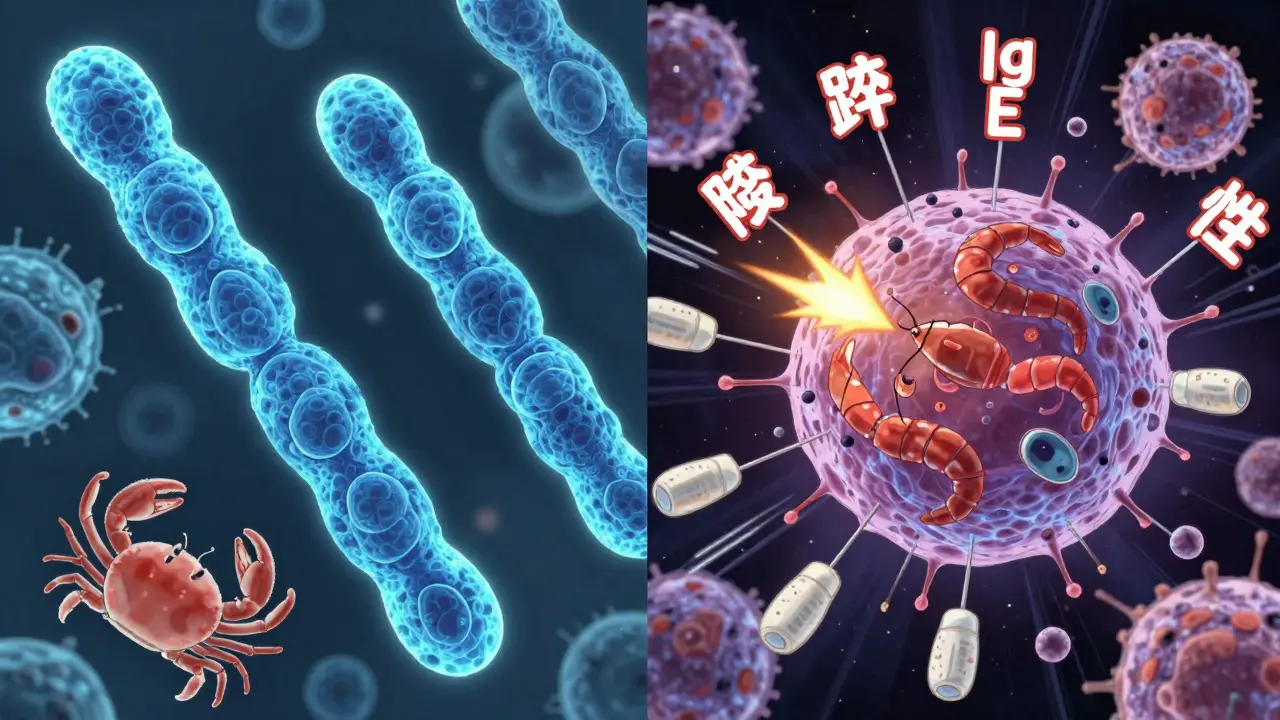
Shellfish allergy isn’t one thing. It’s a web of overlapping immune responses tied to a single protein: tropomyosin. This protein is found in the muscles of shrimp, crab, lobster, and crayfish - and it’s incredibly stable. Unlike many food proteins that break down when cooked, tropomyosin survives boiling, frying, and grilling. That means even well-cooked shellfish can trigger a reaction.What makes this worse is that tropomyosin looks almost identical in all crustaceans. Studies show a 95-100% match in amino acid structure between shrimp, crab, and lobster. That’s why if you’re allergic to one, you’re likely allergic to the others - about 75% of the time. But mollusks like clams, oysters, and mussels? They’re different. Their tropomyosin structure varies enough that only 15-20% of people allergic to shrimp react to them. So if you’ve had a reaction to shrimp but never tried mussels, you might be safe - but you won’t know until you test.
And then there’s the dust mite connection. Dust mites are tiny bugs in your bedding and carpets. They also contain tropomyosin. In fact, the protein is so similar to shellfish tropomyosin that your immune system can’t tell them apart. About 40-50% of people with dust mite allergies test positive for shellfish allergy on blood tests - even if they’ve never eaten shellfish. This leads to false positives. A 2025 study found that nearly 68% of people with dust mite sensitization had positive IgE results for shellfish, but only a small fraction actually had symptoms. That’s why doctors now recommend component-resolved diagnostics - testing specifically for tropomyosin, not just a general shellfish extract. If your IgE is only reacting to dust mite-like proteins, you might not need to avoid all shellfish.
What You’re Really Allergic To: Beyond Tropomyosin
Tropomyosin is the main villain, but it’s not the only one. Other proteins in shellfish can also trigger reactions:- Sarcoplasmic calcium-binding protein (SCBP): Found in shrimp, this triggers reactions in 85% of allergic children.
- Arginine kinase: Also heat-stable and common in crustaceans.
- Myosin light chain and hemocyanin: Less common, but still capable of causing severe reactions.
Here’s the practical takeaway: if you’ve had a reaction to shrimp, you’re probably reacting to tropomyosin. But if your reaction was mild - maybe just a stomach ache or a rash - you might not be allergic to all shellfish. A blood test that checks for specific proteins can tell you whether you’re truly allergic to shrimp, or if you’re just cross-reacting to dust mites. The combination of tropomyosin and SCBP testing gives doctors a 92% accuracy rate in predicting true shrimp allergy. That’s far better than the old method of testing for “shrimp extract,” which gave false positives in up to 60% of cases in high-dust-mite areas like Sydney, Singapore, or coastal California.
Dining Out: The Real Danger Isn’t What’s on the Menu
You might think the biggest risk is ordering something with shrimp in it. But here’s the truth: 87% of shellfish reactions happen in seafood restaurants. Why? Because cross-contact is everywhere.Shared fryers are the silent killer. A 2019 study found that 63% of crustacean reactions from dining out came from oil used to fry both fish and shrimp. Even if your dish doesn’t have shellfish, if it was fried in the same oil as shrimp, you’re at risk. Same goes for grills, cutting boards, tongs, and even the chef’s hands. A 2023 survey of restaurant staff showed that only 37% of servers could correctly identify shellfish ingredients on a menu - and most didn’t know the difference between “shellfish-free” and “no shellfish added.”
Asian restaurants are especially risky. Soy sauce, fish sauce, oyster sauce, and even some broths contain hidden shellfish. A 2020 case series documented dozens of reactions from dishes labeled “vegetarian” or “chicken” that had shellfish extract in the seasoning. Language barriers make it worse - 32% of reactions at ethnic restaurants happened because the staff didn’t understand the severity of the allergy.
How to Eat Out Without Fear
You don’t have to give up dining out. But you need a system.- Call ahead - 24 hours before. Don’t just ask if they have “shellfish-free” options. Ask: “Do you use the same fryer for shrimp and other foods?” “Do you use oyster sauce in your stir-fries?” “Can I speak to the chef?” Restaurants that take this seriously will have a plan.
- Use a chef card. The Food Allergy Research & Education (FARE) chef card is used by over 250,000 people. It’s printed in 15 languages and lists exactly what to avoid: “I am allergic to shrimp, crab, lobster, and all shellfish. Cross-contact with these foods can cause a life-threatening reaction. Please use clean utensils, pans, and oil.”
- Avoid seafood restaurants. Seriously. If you want sushi, go to a place that doesn’t serve shellfish at all. If you want Thai food, find one that uses coconut milk instead of fish sauce.
- Use AllergyEats or Nosh List. These apps let you search for restaurants reviewed by other people with shellfish allergies. Users rate kitchens based on how seriously they take allergies. Nosh List has over 120,000 user reports - and it’s growing.
- Always carry two epinephrine auto-injectors. Even if you’ve never had a severe reaction, shellfish allergy can get worse with each exposure. Don’t wait for a hospital to be nearby.

What’s New in Diagnosis and Treatment
The game is changing. In 2024, the FDA approved a new diagnostic panel called ImmunoCAP ISAC 112. It tests for 112 different allergens at once - including tropomyosin from shrimp, crab, and dust mites - and tells you exactly which protein you’re reacting to. This isn’t just about avoiding food. It’s about avoiding unnecessary restrictions. If your test shows you’re only allergic to dust mite tropomyosin, you might be able to eat scallops safely.And there’s hope on the horizon. In January 2024, a Phase 2 trial at Mount Sinai showed that 70% of participants with shrimp allergy became desensitized after 6 months of daily oral peptide therapy. It’s not a cure, but it means they could tolerate small amounts without reacting. This treatment is still experimental, but it’s the first real progress in decades.
Meanwhile, AI tools like AllergyMapper (launched in March 2024) scan restaurant menus and flag hidden shellfish ingredients. It’s not perfect - it’s 85% accurate - but it’s better than guessing.
What You Should Do Right Now
If you think you have a shellfish allergy:- See an allergist who uses component-resolved testing - not just a general shellfish IgE test.
- Get tested for dust mite allergy. If you’re positive, your shellfish test might be a false alarm.
- Carry your epinephrine. Always.
- Download a FARE chef card and save it to your phone.
- Start using AllergyEats or Nosh List to find safe restaurants near you.
Shellfish allergy doesn’t have to mean isolation. It means awareness. With the right tools, you can eat out, travel, and live without fear - as long as you know what you’re really allergic to, and who you’re talking to in the kitchen.

Faisal Mohamed
January 26, 2026 AT 02:32Bro, tropomyosin is the real MVP of food allergies 🤯. It’s like the universal adapter that turns shrimp, dust mites, and your grandma’s carpet into biological nukes. I had a positive IgE for shellfish for years-turned out I was just allergic to my bed. Component-resolved diagnostics saved my life (and my sushi habit). Now I eat scallops like a boss. 🍤😎
eric fert
January 27, 2026 AT 05:04Let’s be real-this whole ‘shellfish allergy’ narrative is a glorified case of overdiagnosis fueled by pharmaceutical greed and overzealous allergists. You’re telling me that because I’m sensitive to dust mites, I can’t eat lobster? That’s like saying if you’re allergic to cat dander, you can’t eat beef because cows graze in the same fields. The 68% false positive rate? That’s not science-it’s a statistical circus. And don’t get me started on ‘AllergyMapper’-an AI that’s 85% accurate? That’s worse than my ex’s texting habits. We’re pathologizing normal immune variation, folks. 🤷♂️
Aishah Bango
January 29, 2026 AT 03:58People who eat at seafood restaurants without disclosing their allergy are putting others at risk. It’s not just about you-it’s about the chef who has to clean everything with bleach after you leave, the server who doesn’t know what ‘cross-contact’ means, and the kid with anaphylaxis sitting two tables over. If you’re not willing to carry epinephrine or call ahead, you don’t deserve to eat out. Period. 🚫
SWAPNIL SIDAM
January 30, 2026 AT 18:28Wow. This is so important. I have friend in Mumbai-his wife allergic to shrimp. She never knew why she got sick after eating ‘chicken curry’. Turns out, the restaurant uses shrimp paste in everything. Now she carries chef card. Life changed. 🙏
Sally Dalton
February 1, 2026 AT 08:13Okay I just read this and cried a little?? Like I had no idea about the dust mite thing!! I thought I was just ‘sensitive’ to seafood but turns out I’ve been avoiding everything for nothing?? I’m going to my allergist next week and I’m bringing this article with me!! Thank you for writing this so clearly!! 💕
Mohammed Rizvi
February 3, 2026 AT 06:38So you’re telling me the reason I can’t eat crab is because I’m allergic to my couch? That’s the funniest and scariest thing I’ve heard all year. Meanwhile, my cousin in Kerala eats raw oysters for breakfast and still runs marathons. Evolution is weird, folks.
Curtis Younker
February 4, 2026 AT 23:55Guys, this is LIFE-CHANGING info. I used to panic every time I went to a Thai place. Now I call ahead, ask about the oyster sauce, and even show the chef the FARE card. I just had the best pad thai of my life-no hives, no panic, just joy. You don’t have to give up food-you just have to be smart. Start today. You got this. 💪🔥
Napoleon Huere
February 6, 2026 AT 18:45There’s a philosophical layer here beyond immunology. We’re living in an age where our bodies are misreading the world. Dust mites-tiny, invisible, ancient-triggering reactions to creatures we’ve hunted for millennia. Is this evolution? Or is it a cosmic glitch? Tropomyosin doesn’t care about our borders, our menus, or our allergies. It just is. Maybe the real allergy is to the illusion of control. 🌌
Robin Van Emous
February 7, 2026 AT 11:01Thanks for this. I’m from the Philippines and we eat a lot of shrimp. I didn’t know about the dust mite thing. My mom says I’ve always been ‘sick’ after seafood. Now I get it. I’m getting tested next week. Also, I’m printing the chef card. I’m going to show it to my favorite lolo’s restaurant. He’ll understand. He’s old-school. He’ll listen. 🙏
Skye Kooyman
February 9, 2026 AT 04:03Uche Okoro
February 9, 2026 AT 17:01The data presented here is methodologically sound, yet the public health implications remain grossly under-addressed. The conflation of IgE sensitization with clinical allergy represents a paradigmatic failure in allergology. Furthermore, the reliance on self-reported restaurant safety metrics introduces significant selection bias. The absence of longitudinal cohort data undermines the generalizability of the 87% cross-contact statistic. Until we standardize diagnostic protocols across jurisdictions, we risk perpetuating iatrogenic dietary restriction.
Ashley Porter
February 10, 2026 AT 03:19Component-resolved diagnostics are the future. I work in a lab that runs ImmunoCAP ISAC 112. The difference between a positive for tropomyosin vs. a pan-allergen test is night and day. We’ve had patients who avoided seafood for 15 years-turned out they were only reacting to dust mites. They cried when they found out they could eat crab again. This isn’t just science-it’s emotional liberation.
Peter Sharplin
February 11, 2026 AT 13:19As a nurse who’s seen 3 anaphylaxis cases from fried calamari in a non-shellfish restaurant, I can’t stress this enough: shared fryers are the #1 killer. I’ve watched families panic because the server said ‘no shellfish’ but didn’t know what ‘battered’ meant. Always ask: ‘Is this fried in the same oil as shrimp?’ If they hesitate? Walk out. Your life > your craving. And yes-carry two epinephrine pens. Always. I’ve seen people die because they only had one.
shivam utkresth
February 12, 2026 AT 18:12Man, this article hit different. In India, we use shrimp paste in so many things-dosa batter, chutneys, even some curries. My cousin’s wife got sick after eating ‘vegetarian’ dosa. Turns out, the vendor used shrimp stock to ‘enhance flavor’. No one knew. No one told. We need more awareness here. I’m sharing this with my local food bloggers. Maybe we can get a ‘Shellfish-Free’ sticker for restaurants. Simple. Visual. Life-saving. 🇮🇳❤️