When you think of psoriasis, you probably picture red, flaky patches on your elbows or scalp. But for nearly one in three people with this skin condition, the problem runs deeper - straight into the joints. Psoriatic arthritis (PsA) isn’t just a side effect of psoriasis. It’s a full-blown autoimmune disease that attacks both skin and joints, often silently, until the damage is done. If you’ve had psoriasis for years and now wake up with stiff fingers, swollen toes, or lower back pain that doesn’t go away with rest, this isn’t normal aging. It could be PsA.
It Starts With the Skin - But Doesn’t Stop There
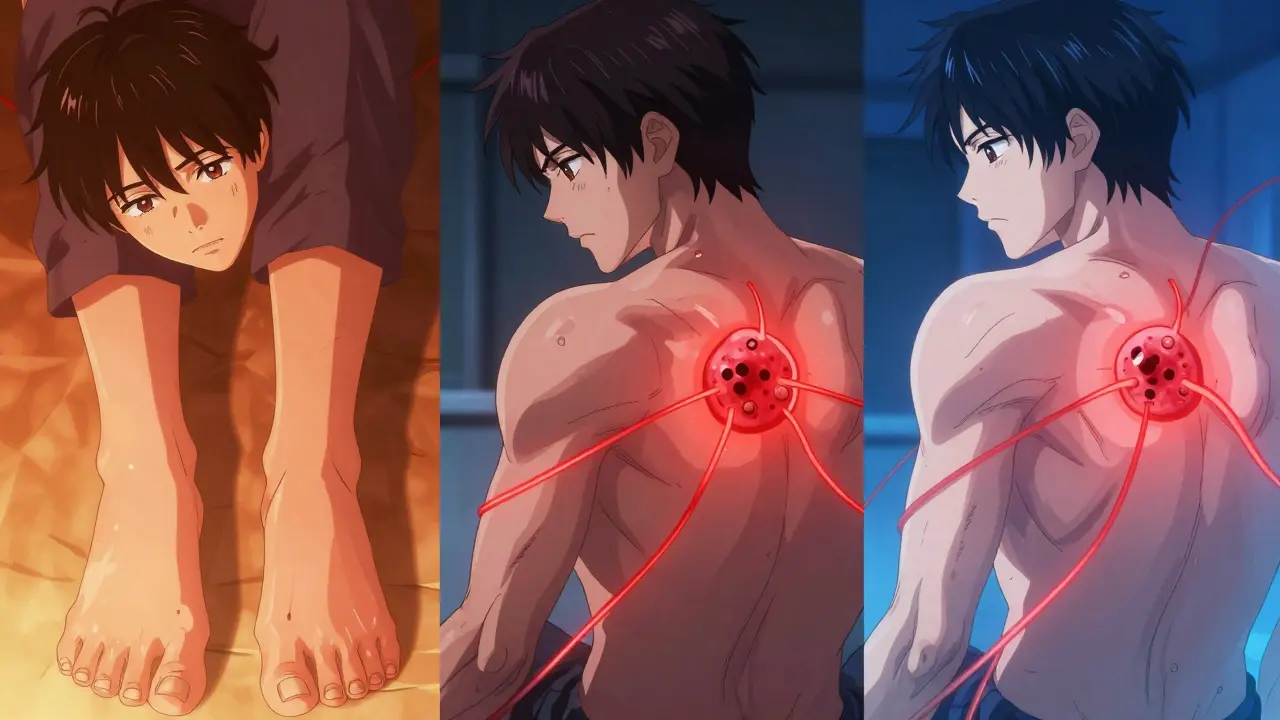
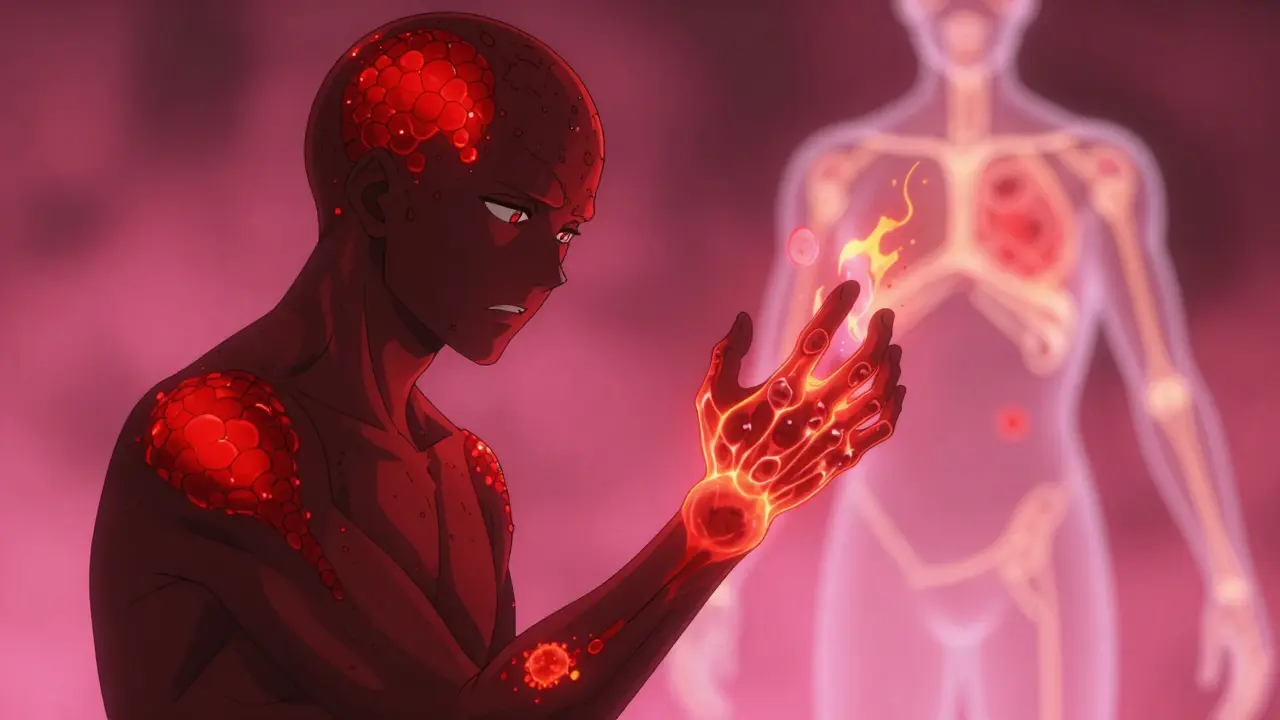
Psoriasis and psoriatic arthritis are two sides of the same coin. Both come from an immune system that’s gone rogue, attacking healthy tissue. In psoriasis, it targets skin cells, causing them to multiply too fast and form thick, scaly plaques. In PsA, the same immune cells turn on the joints, tendons, and even the places where ligaments attach to bone. This isn’t just inflammation. It’s a systemic fire that burns in multiple places at once.Most people develop skin symptoms first. About 85% of PsA cases appear after psoriasis has been present for 5 to 10 years. But here’s the twist: in 15% of cases, joint pain comes first. No rash. No scaling. Just stiff, aching joints. That’s why so many people go years without a diagnosis. They see a rheumatologist for swollen knuckles, a podiatrist for heel pain, or a dermatologist for nail changes - but no one connects the dots.
What Psoriatic Arthritis Actually Feels Like
The symptoms aren’t just "joint pain." They’re specific, unmistakable, and often overlooked.- Dactylitis - Also called "sausage digits," this is when an entire finger or toe swells up like a balloon. It’s not just the joint. It’s the whole digit, inflamed from tendon to bone. About 45% of PsA patients have this. It’s rare in other types of arthritis.
- Enthesitis - Pain where tendons meet bone. Think of the back of your heel (Achilles tendon) or the bottom of your foot (plantar fascia). Walking feels like stepping on glass. This happens in nearly half of PsA cases.
- Nail changes - Pitting, separation from the nail bed, or yellow-brown discoloration. These aren’t just cosmetic. In fact, 80% of PsA patients with nail involvement have them before joint symptoms appear. If your nails look like they’ve been chewed or cracked, it’s a red flag.
- Stiffness that lasts - Morning stiffness in RA usually lasts 30-60 minutes. In PsA, it can last hours. And unlike osteoarthritis, which gets worse with activity, PsA stiffness improves with movement.
One patient from Sydney described it this way: "I thought I had carpal tunnel. Then my toes swelled up. Then my lower back locked up. I went to three doctors before someone asked if I had psoriasis. I hadn’t even noticed the scaling on my scalp."
The Five Faces of Psoriatic Arthritis
PsA doesn’t show up the same way in everyone. It has five distinct patterns:- Asymmetric oligoarthritis - The most common. Affects fewer than five joints, but not the same ones on both sides. Like your left knee and right wrist. Seen in 35-40% of cases.
- Symmetric polyarthritis - Mimics rheumatoid arthritis, with matching joints on both sides. But unlike RA, it rarely causes severe joint destruction. Affects 25-30%.
- Distal interphalangeal predominant (DIP) - Targets the joints closest to the nails. Often paired with nail pitting. Found in 25% of cases. Very rare in other arthritis types.
- Spondylitis - Inflammation in the spine and sacroiliac joints. Causes chronic lower back pain that improves with movement. Affects 5-10%. Often mistaken for mechanical back pain.
- Arthritis mutilans - The rarest and most destructive. Causes bone loss, leading to shortened fingers or toes. Sometimes called "opera glass hand" because the fingers collapse inward. Affects less than 5%.
Knowing which type you have matters. Treatment changes. Prognosis changes. And it’s not always obvious from the start.
How PsA Differs From Other Arthritis Types
It’s easy to confuse PsA with other joint diseases. Here’s how to tell them apart:| Feature | Psoriatic Arthritis | Rheumatoid Arthritis | Osteoarthritis |
|---|---|---|---|
| Joint pattern | Asymmetric (70% of cases) | Always symmetric | Variable, often weight-bearing |
| Rheumatoid factor | Negative | Positive (80%) | Negative |
| Joint damage on X-ray | Pencil-in-cup deformities, new bone growth | Bone erosion, no new bone | Joint space narrowing, bone spurs |
| Skin involvement | Yes (psoriasis) | No | No |
| Nail changes | Common (pitting, separation) | None | None |
| Enthesitis | Very common (35-50%) | Rare | No |
| Systemic inflammation | Yes (affects eyes, gut, heart) | Yes | No |
One key test: if you have psoriasis and your rheumatoid factor is negative, but you have dactylitis or enthesitis - PsA is likely. The combination of nail changes and sausage digits gives an 89% chance of PsA, according to arthritis specialists.
Why Diagnosis Takes So Long - And Why It Matters
The average delay in diagnosing PsA is 2 to 5 years. One study found that patients who waited more than 12 months before getting treatment had over three times more joint damage five years later. Why? Because many doctors still think psoriasis and arthritis are separate issues.Here’s the reality: if you have psoriasis and any of these symptoms - persistent joint stiffness, unexplained fatigue, nail changes, heel pain, or swollen fingers - you need a rheumatologist. Not a general practitioner. Not a dermatologist alone. You need both. Studies show that 82% of patients with optimal outcomes had care from both a dermatologist and a rheumatologist working together.
And it’s not just about pain. PsA increases your risk of heart disease by 2.1 times and raises your chance of developing diabetes by 1.8 times. That’s because chronic inflammation doesn’t stay in the joints. It spreads.
What Works - And What Doesn’t
Treatment has changed dramatically in the last decade. It’s no longer just about painkillers.- DMARDs - Methotrexate is still used in 65% of new cases. It slows progression but doesn’t stop inflammation in many.
- TNF inhibitors - Drugs like adalimumab or etanercept. Work well for 65% of patients within 6 months. But 30% don’t respond.
- IL-17 and IL-23 inhibitors - Newer drugs like secukinumab or guselkumab. The FUTURE 7 trial showed 64% of patients had 50% symptom improvement at 24 weeks. These are now first-line for moderate to severe cases.
- JAK inhibitors - Oral pills like tofacitinib. Fast-acting, but carry increased risk of heart events and cancer. The FDA requires special monitoring.
There’s no one-size-fits-all. Your treatment depends on your subtype, symptoms, and other health risks. If you have spinal involvement, TNF inhibitors work better. If you have nail and skin issues, IL-23 blockers are often more effective.

What Triggers Flares - And How to Control Them
PsA doesn’t flare randomly. There are patterns:- Stress - Cited by 85% of patients. Cortisol imbalance worsens immune overactivity.
- Infections - Especially strep throat. Linked to 1.8 times higher PsA risk within six months.
- Cold weather - 57% report worse symptoms in winter. Likely due to reduced blood flow and increased joint stiffness.
- Obesity - A BMI over 30 triples your risk of developing PsA. Fat tissue produces inflammatory chemicals.
- Joint trauma - If you’ve injured a joint, that’s where PsA is likely to show up. A 4.1-fold increase in risk.
Managing these isn’t optional. Losing 10% of body weight can cut PsA symptoms in half. Reducing stress through sleep, exercise, or mindfulness helps. Avoiding infections means getting flu shots and treating sore throats early.
The Future: Personalized Treatment Is Here
By 2027, doctors will use your genes, proteins, and immune markers to pick your treatment - not guess. Already, trials are showing that patients with certain biomarkers respond better to IL-17 blockers, while others need IL-23 inhibitors. The goal isn’t just to reduce pain. It’s to stop joint damage before it starts.And early action works. The GO-ALIVE study showed that starting biologic therapy within six months of symptoms reduces joint destruction by 73% at two years. That’s the difference between keeping your hands functional and needing surgery.
What to Do Now
If you have psoriasis and joint pain:- See a rheumatologist - even if your dermatologist says it’s "probably nothing."
- Get imaging: X-rays or ultrasound of your hands, feet, and spine.
- Check your nails - pitting or separation is a major clue.
- Track your symptoms: When does stiffness happen? What makes it better or worse?
- Ask for coordinated care - dermatologist + rheumatologist.
You don’t have to live with pain that gets worse over time. PsA is treatable. But only if you catch it early.
Can psoriatic arthritis occur without skin psoriasis?
Yes. About 15% of people develop joint symptoms before any visible skin rash appears. This makes diagnosis harder, but if you have a family history of psoriasis, nail changes, or enthesitis, PsA is still likely. Doctors use blood tests, imaging, and family history to confirm.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint inflammation, RA is symmetric (same joints on both sides) and tests positive for rheumatoid factor. PsA is often asymmetric, has no rheumatoid factor, and includes unique signs like dactylitis and enthesitis. Nail pitting and psoriasis skin lesions are exclusive to PsA.
Can diet or supplements cure psoriatic arthritis?
No cure exists through diet alone. But losing weight, reducing sugar, and avoiding alcohol can cut flare frequency. Omega-3s and vitamin D may help reduce inflammation, but they don’t replace medication. Always discuss supplements with your doctor - some can interfere with biologics.
Does psoriatic arthritis get worse with age?
Not necessarily. PsA doesn’t automatically progress with age. But if left untreated, inflammation continues to damage joints. The key is early, consistent treatment. Many patients who start biologics early stabilize their condition and live without major disability.
Can I still exercise with psoriatic arthritis?
Yes - and you should. Low-impact exercise like swimming, cycling, or yoga improves joint mobility and reduces stiffness. Strength training helps protect joints. Avoid high-impact activities during flares. Always warm up and cool down. Movement is medicine for PsA.
Steph Carr
February 16, 2026 AT 18:51So let me get this straight - you’re telling me my weird nail pitting and that one swollen toe I wrote off as "bad pedicure" is actually my immune system staging a full-on war against my own body? And I thought I was just aging poorly. Thanks for the existential dread, OP. Also - dactylitis? Sausage digits? I’m sending this to my dermatologist with the subject line: "You were right. I’m a walking glitch."