Most people think of opioids as strong painkillers - and they are. But behind that medical use lies a hidden danger: your body can change in ways you don’t expect, and those changes can kill you. It’s not about being weak or making bad choices. It’s about how these drugs work inside your brain and body. Even if you take them exactly as prescribed, your body can build up tolerance, start relying on them to feel normal, and put you at serious risk of overdose.
How Opioids Work - And Why They’re So Dangerous
Opioids like oxycodone, hydrocodone, morphine, and fentanyl bind to special receptors in your brain and spinal cord. These receptors control pain signals, but they also trigger dopamine release - the same chemical involved in pleasure and reward. That’s why opioids don’t just take away pain; they can make you feel calm, even euphoric. It’s a powerful combo: relief plus reward.
But here’s the catch: your brain doesn’t like being flooded with dopamine. Over time, it starts to adapt. The receptors become less sensitive. You need more of the drug to get the same effect. That’s tolerance. And once tolerance sets in, your body starts to depend on the drug just to feel okay. Without it, you get sick - nausea, sweating, muscle aches, anxiety. That’s dependence.
The real danger comes when tolerance doesn’t fully protect you from one life-threatening effect: respiratory depression. Opioids slow your breathing. In high enough doses, they can stop it completely. And here’s the brutal truth: your body builds tolerance to the pain-relieving and euphoric effects faster than it does to the breathing-suppressing effects. So even if you’ve been taking high doses for months, your body hasn’t fully adjusted to the risk of stopping breathing. That’s why overdose can happen at any time - even to someone who’s been using for years.
Tolerance Isn’t Just a Number - It’s a Trap
Let’s say you broke your leg and were prescribed oxycodone. After a week, the same dose doesn’t help as much. Your doctor increases it. Then again. And again. That’s the medical path. But it’s also the path to addiction. Studies show that within six months of chronic opioid use, most patients need 25-50% more medication just to get the same pain control.
What’s worse? That escalating dose doesn’t make you safer. It makes you more vulnerable. The more you take, the more your brain rewires itself. You start needing the drug not just for pain, but to avoid withdrawal. And when you’re stuck in that cycle, you’re no longer using it to feel better - you’re using it just to feel normal.
And then there’s fentanyl. It’s 50 to 100 times stronger than morphine. A few milligrams can kill. Illicit fentanyl is now mixed into counterfeit pills sold as oxycodone or Xanax. People think they’re taking a regular painkiller. They’re not. They’re taking a lethal dose. In 2021, synthetic opioids like fentanyl were involved in over 70% of all opioid overdose deaths in the U.S. - up from just 20% in 2015.
Dependence Isn’t Addiction - But It Can Lead to It
Many people confuse dependence with addiction. They’re not the same thing. Dependence means your body has adapted to the drug. You’ll have withdrawal symptoms if you stop. Addiction is when you keep using despite harm - lost jobs, broken relationships, health problems. You can be dependent without being addicted. But addiction almost always involves dependence.
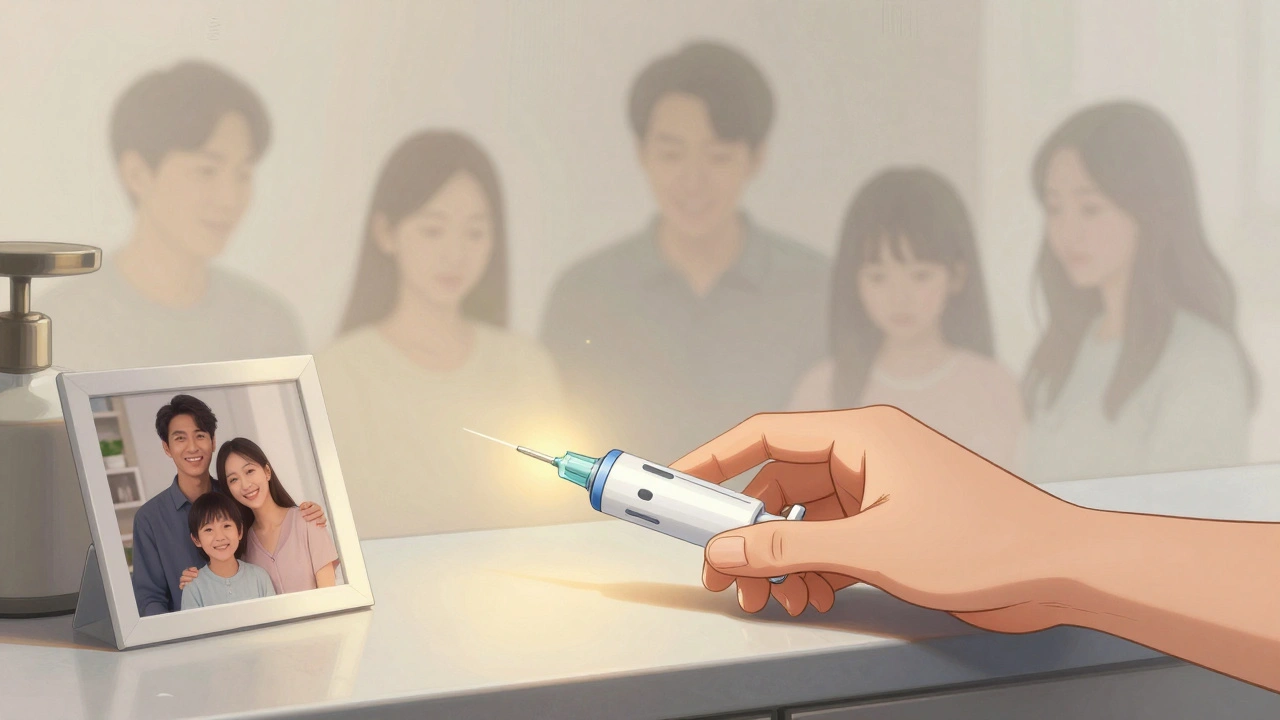
The problem is, once dependence sets in, the line blurs. You start prioritizing the drug. You hide your use. You lie. You might steal. You might turn to street drugs because your prescription ran out. That’s when the risk of overdose spikes - especially if you’re using alone, or mixing opioids with alcohol, benzodiazepines, or sleep aids. These combinations can shut down breathing even faster.

The Relapse Trap: Why Former Users Are at Highest Risk
Here’s one of the most dangerous myths: if you’ve been clean for a while, you’re safe. You’re not.
When you stop using opioids, your body slowly loses its tolerance. Your brain resets. That’s a good thing - it means you’re healing. But if you relapse and take the same dose you used before, your body can’t handle it anymore. You’re not the same person you were six months ago. Your tolerance is gone. Your risk of overdose is sky-high.
Studies show that 65% of opioid overdose deaths happen in people who had previously been treated for opioid use disorder. One Reddit user wrote: “After six months clean, I used my old dose. Paramedics said I was clinically dead for four minutes.” That’s not rare. Harm reduction groups report that 87% of the overdose reversals they’ve handled since 2018 involved people who had been sober for weeks or months.
This is why naloxone - the overdose reversal drug - is so critical. If you or someone you know has ever used opioids, even once, keep naloxone on hand. It’s safe, easy to use, and can bring someone back from the brink. In communities where naloxone is widely distributed, fatal overdoses have dropped by 34%.
Why Some Opioids Are Safer Than Others
Not all opioids are created equal. Buprenorphine, for example, is a partial agonist. It activates opioid receptors - but only up to a point. That means it relieves pain and cravings, but it doesn’t cause the same level of respiratory depression as full agonists like fentanyl or heroin. It has a built-in safety ceiling.
That’s why buprenorphine is a cornerstone of Medication-Assisted Treatment (MAT). When used correctly, it reduces overdose risk by 50%. Since 2023, U.S. doctors no longer need special certification to prescribe it. That’s a big deal. It means more people can get access to this life-saving treatment.
Methadone also helps, but it’s trickier. It’s a full agonist, so it carries overdose risk - especially if misused or mixed with other depressants. But for people with severe dependence, it can be a lifeline. The key is medical supervision.
What You Can Do - Even If You’re Not Using
You don’t have to be someone with a substance use disorder to be at risk. Maybe you’re taking opioids for chronic back pain. Maybe your parent or partner is. Maybe you’ve seen a friend struggle. Here’s what matters:
- If you’re prescribed opioids, ask: “Is this really necessary? Are there alternatives?” Physical therapy, NSAIDs, and nerve blocks can work for many types of pain.
- If you’re on them long-term, talk to your doctor about tapering. Don’t stop cold turkey - that’s dangerous. A slow, supervised reduction is safer.
- Keep naloxone in your home. It’s available over the counter in many pharmacies. Learn how to use it. Teach your family.
- If someone you know is using opioids, don’t shame them. Offer support. Help them find treatment. Carry naloxone with you when you’re together.
- Never use alone. If you’re using opioids recreationally, always have someone with you who knows how to respond to an overdose.
The Bigger Picture: Why This Crisis Keeps Growing
The opioid crisis didn’t happen overnight. In 2012, doctors in the U.S. wrote over 81 prescriptions for every 100 people. That’s nearly one per person. By 2021, that number dropped to 47 - thanks to better guidelines and awareness. But as prescriptions fell, illicit fentanyl surged. Drug dealers didn’t care about pain relief. They cared about profit. Fentanyl is cheap to make. A tiny amount goes a long way. So they started cutting it into heroin, cocaine, and fake pills.
The result? More deaths. More families shattered. More people trapped in a cycle they didn’t choose.
But there’s hope. The NIH has invested $1.5 billion into finding non-addictive pain treatments. New drug formulations are being developed to block abuse without reducing pain relief. And more doctors are now able to prescribe buprenorphine. The goal isn’t to punish people - it’s to save lives.
The truth is, opioids are powerful tools. But they’re not magic. They come with costs - physical, emotional, and sometimes fatal. Understanding tolerance, dependence, and overdose isn’t about fear. It’s about respect. Respect for the drug. Respect for your body. And respect for the people who love you.
Can you become dependent on opioids even if you take them exactly as prescribed?
Yes. Dependence is a physical adaptation your body makes in response to regular opioid use - even when taken exactly as directed by a doctor. It doesn’t mean you’re addicted. But it does mean that if you stop suddenly, you’ll likely experience withdrawal symptoms like nausea, sweating, anxiety, and muscle pain. That’s why doctors recommend tapering off slowly under medical supervision.
Why do people overdose even after years of using opioids?
Because tolerance to the pain-relieving and euphoric effects develops faster than tolerance to respiratory depression. Even long-term users don’t fully adapt to the drug’s ability to slow breathing. So if they take a higher dose, use a stronger opioid like fentanyl, or mix it with alcohol or sedatives, their breathing can stop. That’s why overdose can happen at any stage - even to experienced users.
Is fentanyl the main cause of opioid overdose deaths today?
Yes. In 2021, synthetic opioids - mostly fentanyl and its analogs - were involved in 70.3% of all opioid-related overdose deaths in the U.S. Unlike prescription opioids, illicit fentanyl is often mixed into other drugs without the user’s knowledge. A single pill or dose can contain a lethal amount. That’s why overdose deaths have surged even as prescription rates have fallen.
Can naloxone save someone who overdoses on fentanyl?
Yes. Naloxone works by rapidly blocking opioid receptors in the brain, reversing the effects of overdose - including from fentanyl. Because fentanyl is so potent, multiple doses of naloxone may be needed. But it still works. Naloxone is safe, easy to use, and has no effect if opioids aren’t present. Keeping it on hand - and knowing how to use it - can save a life.
Why are people who’ve been clean at higher risk of overdose if they relapse?
When someone stops using opioids, their body gradually loses tolerance. Their brain resets. But their cravings and habits may still be there. If they relapse and take the same dose they used before quitting, their body can’t handle it. That’s why overdose deaths are highest among people returning to use after a period of abstinence. This is why harm reduction programs emphasize starting with a much smaller dose after recovery.
Is buprenorphine safer than other opioids for treating dependence?
Yes. Buprenorphine is a partial opioid agonist, meaning it activates opioid receptors but only up to a certain point. This creates a ceiling effect - it reduces cravings and withdrawal without causing the same level of respiratory depression as full agonists like heroin or fentanyl. It’s also less likely to be misused and has a lower risk of fatal overdose. That’s why it’s a first-line treatment for opioid use disorder.
What Comes Next
If you’re on opioids - whether by prescription or not - the most important thing is awareness. You don’t need to panic. But you do need to understand the risks. Talk to your doctor. Ask about alternatives. Ask about naloxone. Ask about tapering. If you’re helping someone else, don’t wait for a crisis. Learn the signs of overdose. Keep naloxone nearby. Be the person who knows what to do.
There’s no shame in needing help. There’s no shame in asking for it. And there’s no shame in saving a life.

Shayne Smith
December 5, 2025 AT 21:57Just saw this and had to say thanks. My cousin OD’d last year after being clean for 8 months. Naloxone saved him. I keep two in the house now.
Brooke Evers
December 6, 2025 AT 22:23I’ve been a nurse for 18 years and I’ve seen this play out too many times. People think tolerance means they’re ‘used to it’ - but it’s not about habit, it’s about biology. Your brain literally forgets how to breathe without the drug. I had a patient who’d been on oxycodone for five years after a back surgery. He took his normal dose one night. Didn’t wake up. His wife found him. He was blue. We got him back with three doses of naloxone. He’s alive now. But he’ll never take another opioid. Not because he’s weak - because he learned how cruel this drug can be. And honestly? Most doctors don’t explain this part. They just write the script. No one tells you that your body’s ability to adapt to pain relief outpaces its ability to adapt to respiratory depression. That’s the trap. You think you’re safe because you’ve been doing it for years. But your body isn’t keeping up. And one day, it catches up with you - in the worst way possible.
Saketh Sai Rachapudi
December 8, 2025 AT 07:16Indians dont do this shit. We dont get addicted to pills. We got real painkillers like masala chai and yoga. This is a white people problem. Stop pushing your drugs on the world.
joanne humphreys
December 9, 2025 AT 21:21I appreciate how clearly this breaks down the difference between dependence and addiction. I’ve seen friends labeled as addicts when they were just dependent after surgery. The stigma makes it harder to seek help. I also didn’t know buprenorphine didn’t need special certification anymore - that’s huge. More doctors need to know this. And naloxone should be as common as aspirin. I’ve started carrying it in my purse since my brother’s friend overdosed last winter. It’s not about judgment. It’s about being prepared.
Nigel ntini
December 9, 2025 AT 23:27Excellent, thoughtful post. The point about relapse being the deadliest moment is critically under-discussed. Many recovery programs focus on abstinence but neglect the physiological reality of lost tolerance. A person who’s been sober for six months and takes their old dose is essentially a first-time user with the same cravings. That’s not weakness - it’s neurobiology. We need public health campaigns that emphasize this. Not just ‘don’t use’ but ‘if you relapse, start with 1/4 of your old dose’. And yes - naloxone should be sold next to condoms in pharmacies. Simple, effective, life-saving. Why isn’t it?
Mansi Bansal
December 10, 2025 AT 18:57It is my profound conviction, grounded in empirical observation and sociological analysis, that the opioid epidemic is a direct consequence of the erosion of traditional moral frameworks in Western societies, coupled with the commodification of pharmaceuticals by corporate entities operating under a neoliberal economic paradigm. The individual, stripped of spiritual resilience and communal accountability, becomes susceptible to chemical escapism - a symptom, not a cause. Furthermore, the normalization of pharmacological intervention for non-terminal pain reflects a pathological aversion to suffering, which, historically, was regarded as a crucible for character formation. The proliferation of naloxone, while ostensibly benevolent, may inadvertently perpetuate a cycle of dependency by mitigating the natural consequences of deviant behavior. One must ask: Are we saving lives, or merely postponing accountability?
pallavi khushwani
December 11, 2025 AT 17:38i used to think if you take meds like your supposed to you’re fine… until my dad started shaking every time he missed a dose. he never did drugs, never got high. just had bad back pain. now he’s on buprenorphine and says it’s the first thing that didn’t make him feel like a zombie. i’m glad there’s a safer way. we all just want to feel okay.
Billy Schimmel
December 13, 2025 AT 07:43So… you’re saying if I take a pill and feel good, I’m just one bad day away from dying? Cool. Thanks for the reminder.
brenda olvera
December 14, 2025 AT 19:25My aunt took opioids for arthritis and ended up in rehab. She says the worst part wasn’t the withdrawal - it was the guilt. Like she failed because her body changed. But it wasn’t her fault. It’s the drug. Not her. We need to stop blaming people and start fixing the system
Ibrahim Yakubu
December 16, 2025 AT 17:00They say fentanyl is killing people but who’s really behind this? Big Pharma, the DEA, the WHO - all working together to depopulate the lower classes. You think this is about pain? It’s about control. They want you dependent on pills so you won’t question the system. And now they’re pushing naloxone like it’s a cure - but it’s just another tool to keep you alive while they keep feeding you poison. Wake up.
Chris Park
December 17, 2025 AT 19:40Actually, the real cause of opioid deaths is the illegalization of heroin in the 1970s. If we had just regulated it like alcohol, people wouldn’t be getting fentanyl-laced pills. This whole war on drugs is a scam. The government created the crisis so they could profit from rehab centers and prison contracts. Naloxone? Just a PR stunt to make people think they’re doing something. Meanwhile, the real solution - legal, regulated opioids - is still banned.