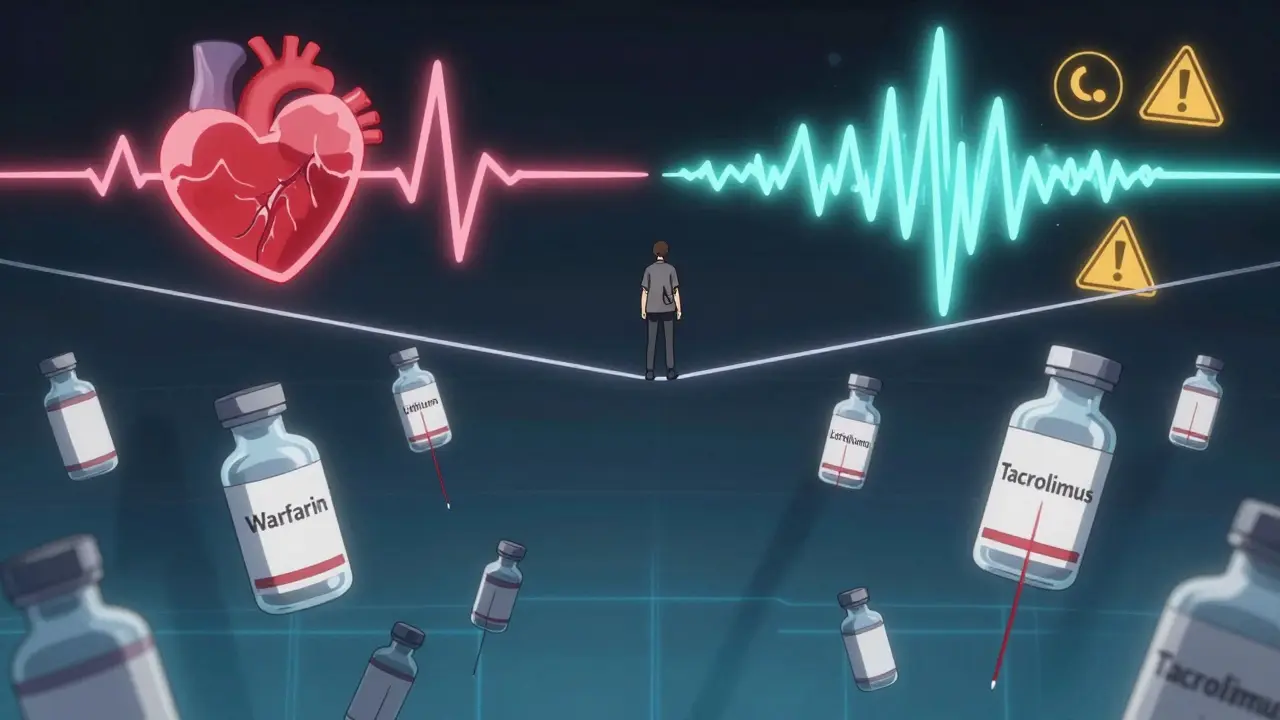
When a medication has a narrow therapeutic index, even a tiny change in dose can turn treatment into danger. These aren’t just any pills - they’re the ones where 5% more could mean a stroke, 5% less could mean a seizure, and switching brands might throw your whole system off balance. If you’re taking one of these drugs, you’re not just following a prescription - you’re walking a tightrope. And that’s why knowing which drugs fall into this category isn’t optional - it’s life-saving.
What Makes a Drug ‘Narrow Therapeutic Index’?
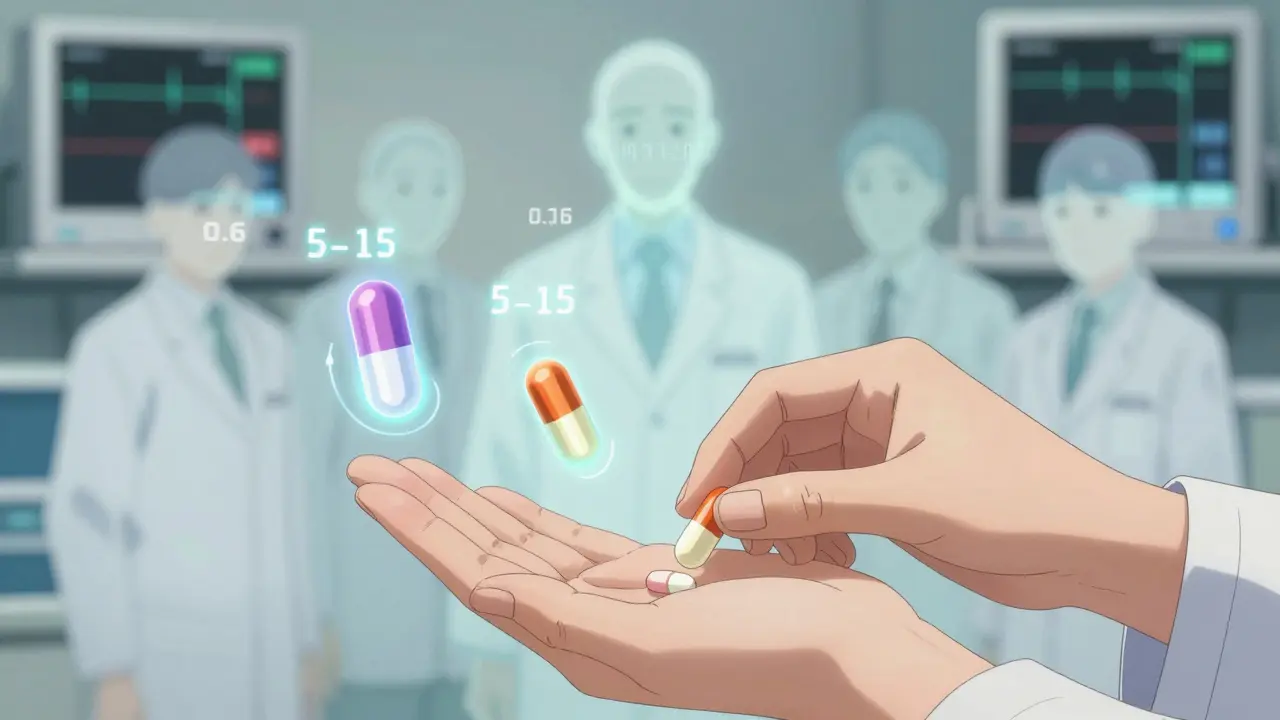
NTI stands for Narrow Therapeutic Index. Simply put, it means the difference between a dose that works and a dose that harms is razor-thin. For most drugs, your body can handle some variation - a missed pill, a slightly higher dose, even a different generic brand. But with NTI drugs, that margin of error is often less than 20%. The U.S. Food and Drug Administration defines them as medications where small changes in blood concentration can lead to serious side effects or treatment failure - think organ rejection, toxic poisoning, or uncontrolled seizures.
How thin is this line? Take digoxin, a heart medication. Its therapeutic range? 0.5 to 2.0 nanograms per milliliter of blood. That’s less than a drop in a swimming pool. Go above 2.0? You risk deadly heart rhythms. Drop below 0.5? Your heart failure could worsen. This isn’t theoretical. Studies show that a 10% dose increase in warfarin can push INR levels from safe (2.5) into dangerous territory (over 4.0), increasing bleeding risk by more than seven times.
The Core NTI Drug List You Need to Know
There’s no single official global list, but based on FDA guidance, state pharmacy boards, and clinical guidelines, these are the most common NTI drugs you’ll encounter in practice:
- Warfarin - The classic anticoagulant. Its therapeutic window is measured by INR (International Normalized Ratio). Target range: 2.0-3.0 for most conditions. Above 4.0? High risk of internal bleeding. Below 1.5? Risk of clotting.
- Digoxin - Used for heart failure and atrial fibrillation. Therapeutic range: 0.5-2.0 ng/mL. Toxicity can cause nausea, confusion, and fatal arrhythmias.
- Lithium - A mood stabilizer for bipolar disorder. Therapeutic level: 0.6-1.2 mmol/L. Levels above 1.5 can cause tremors, kidney damage, or coma. Even slight dehydration can spike levels.
- Phenytoin - An anticonvulsant. Therapeutic range: 10-20 mcg/mL. Too low? Seizures return. Too high? Slurred speech, dizziness, and permanent nerve damage.
- Tacrolimus - A transplant immunosuppressant. Trough levels must stay between 5-15 ng/mL. A drop below 5? Risk of organ rejection. Above 15? Kidney failure and neurotoxicity.
- Carbamazepine - Another seizure drug. Range: 4-12 mcg/mL. Levels above 12 can cause liver toxicity and bone marrow suppression.
- Valproic acid - Used for seizures and bipolar disorder. Therapeutic range: 50-100 mcg/mL. High levels cause pancreatitis and liver failure.
- Cyclosporine - Another transplant drug. Target: 100-400 ng/mL. Small fluctuations can mean the difference between organ survival and rejection.
- Levothyroxine - Thyroid hormone replacement. While not always measured by blood levels, even minor changes in brand or formulation can shift TSH levels dramatically - from normal (1.2) to severely elevated (8.7), as seen in real cases.
- Sirolimus - Used in transplant patients and some cancers. Therapeutic range: 5-15 ng/mL. Similar to tacrolimus, precision matters.
- Aminoglycosides (e.g., Gentamicin) - Antibiotics with high kidney and ear toxicity. Peak levels must be 5-10 mcg/mL; troughs must stay under 2 mcg/mL to avoid permanent hearing loss.
Why Generic Substitutions Can Be Risky
Many people assume generics are interchangeable. With NTI drugs, that’s not true. The FDA requires stricter bioequivalence standards for these drugs: 90% confidence intervals for absorption must fall between 90% and 111.11% of the brand-name drug. For non-NTI drugs, the range is 80%-125%. That might sound minor, but for someone on tacrolimus after a heart transplant, even a 5% difference in absorption can trigger rejection.
Real-world examples aren’t rare. In 2023, a Reddit thread from a pharmacist detailed how switching a 62-year-old patient from branded to generic levothyroxine caused TSH to jump from 1.2 to 8.7 - a sign of severe under-treatment. It took three months and five dose adjustments to stabilize. That’s not a fluke. In 47 U.S. states, pharmacists are legally required to get explicit permission from the prescribing doctor before substituting an NTI drug. Some states, like North Carolina and Oklahoma, have published official lists of which drugs require this.
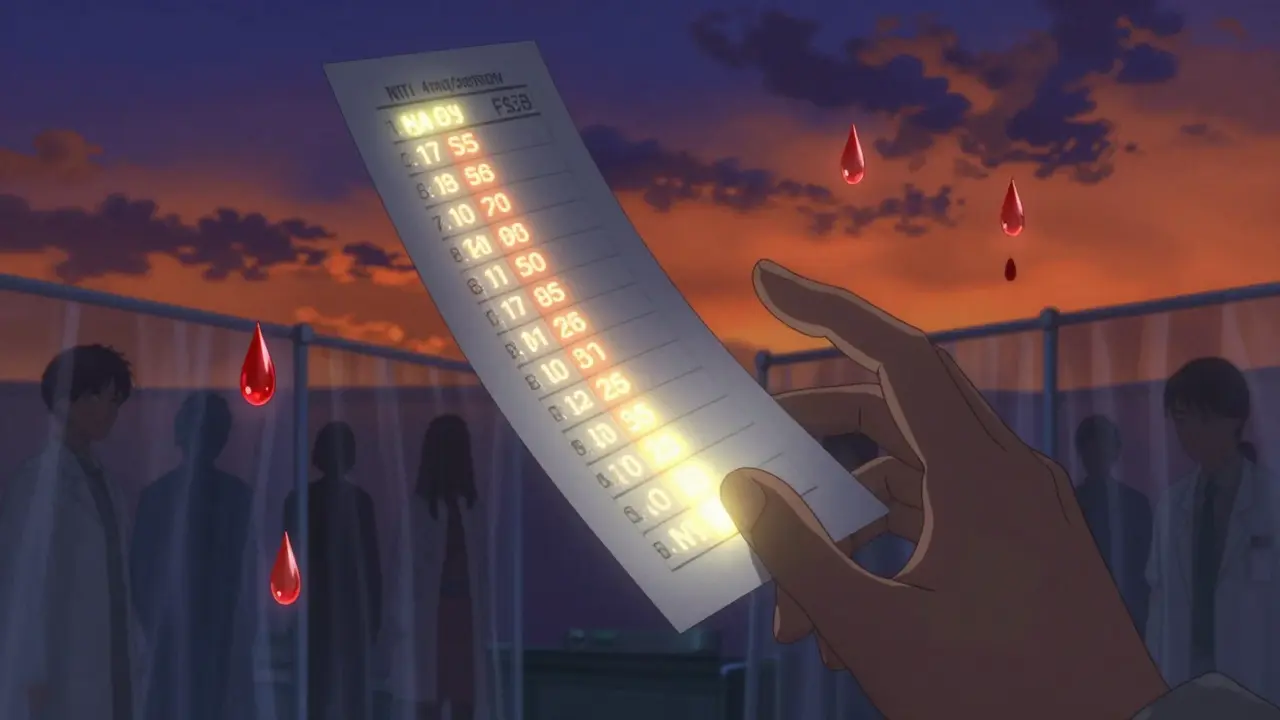
Monitoring: The Lifeline for NTI Drug Safety
You can’t just take an NTI drug and forget about it. Regular monitoring isn’t optional - it’s part of the treatment.
- Warfarin: INR checks every 3-5 days when starting, then weekly until stable.
- Lithium: Blood tests every 3-6 months, but more often if you’re sick, dehydrated, or starting a new medication.
- Phenytoin: Trough levels checked monthly, or after any dose change.
- Tacrolimus: Trough levels measured 3 times a week during initial treatment, then weekly or biweekly.
- Levothyroxine: TSH tested every 6-8 weeks after a dose change, then every 6-12 months if stable.
Yet, adherence is poor. One study found 32% of lithium patients miss their monitoring appointments. Only 45% of hospital systems have automated alerts when levels go out of range. That means a lot of patients are flying blind - and that’s how preventable harm happens.
Emerging NTI Drugs: The New Frontier
The list isn’t static. New targeted cancer drugs are joining it. Axitinib, ponatinib, and olaparib - used for advanced cancers - now have defined therapeutic ranges. For example, ponatinib’s target is 20-50 ng/mL. Too low? Cancer progression. Too high? Severe liver damage or blood clots.
The FDA is now reviewing whether newer anticoagulants like apixaban and rivaroxaban should be added to the NTI list. While they’re considered safer than warfarin, their narrow window for bleeding risk means even small dosing errors can be catastrophic. This reflects a broader trend: precision medicine is creating more NTI drugs, not fewer.
What You Should Do
If you’re prescribed an NTI drug:
- Know the name of your drug and its therapeutic range. Ask your doctor or pharmacist.
- Never switch brands without talking to your prescriber - even if it’s labeled “generic.”
- Keep a log of your blood test results. Don’t rely on memory.
- Report side effects immediately - even small ones like a slight tremor or unexplained bruising.
- Ask if your pharmacy has a system to flag NTI drug substitutions.
For caregivers and family members: If someone you care for is on one of these drugs, help them track appointments and medication changes. These drugs don’t just affect the patient - they affect everyone around them.
Why This Matters More Than You Think
NTI drugs make up only about 15% of medications requiring blood monitoring - but they cause 30% of dosing-related adverse events. That’s not a coincidence. It’s a warning. As more targeted therapies enter the market, this category will only grow. The future of safe medication use isn’t just about prescribing the right drug - it’s about knowing exactly how much is safe, how to monitor it, and when to say no to substitutions.
There’s no room for guesswork here. Precision isn’t a buzzword - it’s the difference between life and death.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe - but they must meet stricter FDA standards to be approved for NTI drugs. Some generic versions of drugs like phenytoin and levothyroxine are bioequivalent and safe. However, switching between different generic manufacturers (even for the same drug) can cause fluctuations. Always check with your prescriber before switching, even if the label says "generic."
Can I stop monitoring my NTI drug levels if I feel fine?
No. Feeling fine doesn’t mean your drug level is in range. Many NTI drugs cause no symptoms until toxicity or underdosing becomes severe. Lithium toxicity, for example, can cause confusion and kidney damage before you feel anything. Regular blood tests are the only way to know your levels are safe. Skipping tests increases your risk of serious harm.
Why do some states have different NTI drug lists?
Each state’s pharmacy board sets its own rules based on local prescribing patterns, legal frameworks, and reported adverse events. For example, Oklahoma includes nortriptyline and esketamine on its list because of rising use in depression treatment, while North Carolina focuses on older, well-established NTI drugs like digoxin and warfarin. Always follow your state’s guidelines - they’re based on real patient data.
Do insurance plans cover NTI drug monitoring?
Yes, most insurance plans, including Medicare, cover therapeutic drug monitoring for approved NTI drugs. Medicare covers 80% of the cost for tests like INR, lithium levels, and tacrolimus troughs. However, some labs charge out-of-pocket fees for expedited results. Always ask your pharmacy or lab about costs before testing.
What should I do if my doctor prescribes a new NTI drug?
Ask three things: 1) What’s the target therapeutic range? 2) How often do I need blood tests? 3) Can I stay on the same brand or generic? Write down the answers. Set reminders for your next test. Keep a copy of your last lab result. These drugs require active participation - don’t assume your doctor will remind you. Your safety depends on it.
Next Steps
If you’re on an NTI drug, the next thing you should do is pull out your last blood test report. Look at the numbers. Are they in range? If you’re unsure, call your pharmacist. If you haven’t had a test in over 6 months, schedule one now. If you’ve switched brands recently, talk to your doctor about whether you need a repeat test. Don’t wait for symptoms - by then, it might be too late.
Reggie McIntyre
February 12, 2026 AT 06:38Man, this post hit different. I’ve been on lithium for a decade, and I still get that little chill every time I see my bloodwork numbers. It’s not just medicine-it’s like balancing on a wire made of glass while juggling three flaming torches. One typo in the lab report, one extra cup of coffee, one hot day without drinking enough water-and boom, you’re in the ER. But here’s the thing: knowing this stuff? It’s power. Not fear. Power.
I started keeping a little notebook-dates, doses, how I felt, even the weather. Weird? Maybe. But when my doc asked why my levels spiked last month, I handed him the notebook. He nearly cried. Turns out, I’d been drinking cold brew instead of water. Who knew caffeine and lithium were mortal enemies?
So yeah. This isn’t just a list. It’s a survival guide. And if you’re on one of these meds? You’re not broken. You’re a damn scientist with a pulse.
Carla McKinney
February 12, 2026 AT 23:01The FDA’s 90-111% bioequivalence standard for NTI drugs is a farce. It’s not rigorous enough. Real bioequivalence should be 95-105%. The fact that we’re allowing 111.11% is reckless. I’ve reviewed the data from 2019-2023-there were 147 documented cases of tacrolimus rejection tied to generic switches. That’s not coincidence. That’s negligence. And don’t get me started on levothyroxine. The difference between Synthroid and a generic isn’t pharmacokinetics-it’s corporate greed wrapped in a white pill.
Also, the post mentions monitoring. Fine. But where’s the data on compliance? Only 45% of hospitals have alerts? That’s not a system failure. That’s a societal failure. We’re treating life-threatening conditions like they’re seasonal allergies.
Ojus Save
February 13, 2026 AT 11:33so i read this whole thing and i just wanna say… like… wow. i’m from india and we dont really have this kind of detailed tracking here. my uncle is on warfarin and they just give him a script and say ‘take it daily’. no blood tests, no followups. i think this is insane. but also kinda amazing that u guys have this level of care. maybe we need to copy this. or at least steal the list.
also i typed this on my phone and im sure i messed up some words. sorry.
Jack Havard
February 15, 2026 AT 03:58Let’s be real. This whole NTI thing is a profit machine. Blood tests cost money. Pharmacies make money off monitoring. Labs make money off monitoring. Doctors make money off monitoring. And suddenly, every generic drug is ‘too dangerous’ unless you pay extra. You think the FDA really cares about your lithium levels? Or are they just protecting brand-name manufacturers?
I’ve been on phenytoin for 12 years. Switched generics three times. Never had a seizure. Never had a side effect. My TSH? Stable. My INR? Perfect. So why are we scared? Because the system wants you scared. And scared people pay more.
Stacie Willhite
February 17, 2026 AT 01:21Thank you for writing this. I’m a nurse, and I see how often patients get scared or confused by these drugs. They think, ‘If it’s just a pill, why do I need a blood test every week?’ But you laid it out so clearly. I’ve had patients cry because they didn’t know their levels were dropping-and they thought they were ‘getting better.’ This isn’t just information. It’s peace of mind.
Also, the part about caregivers? So true. My mom’s on tacrolimus. I set her alarms. I call her pharmacy. I print her lab results. She says I’m overbearing. I say I’m her safety net.
Gabriella Adams
February 17, 2026 AT 13:20As a clinical pharmacist, I’ve reviewed over 300 NTI drug cases in the last five years. Let me cut through the noise: generics are not inherently dangerous. But switching between multiple generic manufacturers-without monitoring-is a recipe for disaster. One patient went from Amneal to Teva to Mylan levothyroxine in six months. TSH went from 1.8 to 12.4. She was asymptomatic. Until she wasn’t. Then she had cardiac arrest.
The key isn’t brand loyalty. It’s consistency. Once you find a generic that works, STAY ON IT. Don’t let your pharmacy swap it out unless you give explicit permission. And if your doctor says ‘it’s all the same’? Ask them to look at the bioequivalence data. They might not know it.
Also, yes-insurance covers monitoring. But many patients don’t know how to ask. Tell your pharmacist: ‘I need my NTI drug levels tracked.’ Say it like you mean it. They’ll help you.
steve sunio
February 19, 2026 AT 04:50nti drugs? more like nti scams. i mean come on. if you can't afford to be monitored every week, you shouldn't be on the drug. plain and simple. the system is rigged. people in africa and asia are dying because they can't afford these tests. but here in the usa, we're making it a luxury. what a joke. also, why is levothyroxine even on this list? it's a hormone. not a rocket fuel. fix your healthcare system before you scare people with lists.
athmaja biju
February 20, 2026 AT 22:43India has better drug safety than the U.S. We don’t need 12 blood tests for one pill. Our doctors trust the medicine. Our patients trust their doctors. In America, you’re treated like a lab rat. We have 1.4 billion people and 99% of them take their meds without monitoring. Why? Because we don’t panic. You overthink everything. Your ‘precision medicine’ is just fear marketing. Also, why is tacrolimus listed? We give it to transplant patients with no lab access. They survive. You just need faith.
Robert Petersen
February 21, 2026 AT 18:49This is one of those posts that makes you feel like you’re not alone. I’m on cyclosporine after a kidney transplant. I used to panic every time I got a new bottle-‘Is this the same?’ ‘Did they switch it?’ Then I started asking my pharmacist to write ‘DO NOT SUBSTITUTE’ on the label. Now, they do it automatically. No drama. Just clarity.
And yeah, the monitoring is a pain. But I’ve got a spreadsheet. I color-code my results. Green = good. Yellow = check in. Red = call doc. My wife says I’m obsessed. I say I’m alive. And I’m not taking that for granted.