Migraine vs. Tension Headache Identifier
Migraine Characteristics
Throbbing pain, often one-sided, with nausea, visual aura, and light sensitivity.
Tension Headache Characteristics
Pressing tightness around head, usually mild to moderate, without nausea or aura.
Your Headache Type Analysis
Treatment Recommendations:
- Keep a headache diary to track patterns
- Consider over-the-counter pain relievers
When a pounding ache takes over your head, you’ll want to know whether you’re dealing with a migraine or a tension headache. Knowing the difference can save you time, money, and a lot of frustration. Below you’ll find a clear breakdown of what sets these two common pain types apart, how to spot them, and what works best for relief.
Quick Takeaways
- Migraine pain is usually throbbing, often on one side, and may come with nausea, visual aura, and light sensitivity.
- Tension‑type headache feels like a tight band around the head, is usually mild‑to‑moderate, and rarely includes nausea.
- Triggers differ: migraines react to hormonal shifts, certain foods, and strong smells; tension headaches are linked to stress, poor posture, and muscle strain.
- Acute treatment for migraines often involves triptans, while tension headaches respond well to over‑the‑counter NSAIDs and relaxation techniques.
- Prevention strategies focus on lifestyle: migraine‑specific diets and hormonal tracking versus ergonomic adjustments and stress‑management for tension headaches.
Defining the Two Headaches
Migraine is a neurological disorder characterized by recurring attacks of moderate‑to‑severe headache, usually unilateral, often accompanied by nausea, vomiting, photophobia, and phonophobia. The International Classification of Headache Disorders (ICHD‑3) recognizes several subtypes, the most common being migraine without aura and migraine with aura.
Tension‑type headache (often abbreviated TTH) is classified as a primary headache caused by pericranial muscle tension, presenting as a bilateral, pressing or tightening sensation. It accounts for roughly 70% of all headache visits to primary‑care clinics.
Typical Symptoms and How They Feel
Migraine symptoms tend to unfold in stages:
- Prodrome: subtle changes such as mood swings, food cravings, or yawning 12‑48hours before pain.
- Aura (optional): visual disturbances like scintillating scotomas, zig‑zag lines, or blind spots.
- Headache phase: throbbing pain, often pulsing at 2‑4Hz, localized to one side, lasting 4‑72hours. Nausea, vomiting, sensitivity to light (photophobia) and sound (phonophobia) are common.
- Post‑drome: feeling drained, fuzzy‑headed, or unusually energetic for up to 24hours.
Tension‑type headache symptoms are usually steadier:
- Band‑like pressure or tightness across both temples or the back of the head.
- Mild‑to‑moderate intensity, rarely exceeding 6/10 on a pain scale.
- Absence of nausea, vomiting, or pronounced photophobia/phonophobia.
- Duration can range from 30minutes to several days, often recurring at the same time of day.
Common Triggers
Understanding what sets off each headache type helps you avoid the next attack.
| Migraine Triggers | Tension‑type Triggers |
|---|---|
| Hormonal fluctuations (menstruation, oral contraceptives) | Prolonged sitting or poor ergonomics |
| Specific foods (aged cheese, red wine, MSG) | High stress or emotional tension |
| Sleep deprivation, irregular sleep patterns | Jaw clenching, teeth grinding (bruxism) |
| Bright or flickering lights, strong odors | Cold weather exposure causing neck muscle contraction |
| Physical exertion, especially sudden intense activity | Dehydration (less common but can exacerbate muscle tension) |
Note that some triggers overlap-stress can aggravate both, but the downstream mechanisms differ. In migraines, stress often triggers neurovascular changes; in tension headaches it tightens the scalp‑muscle fascia.
Underlying Mechanisms (Why They Happen)
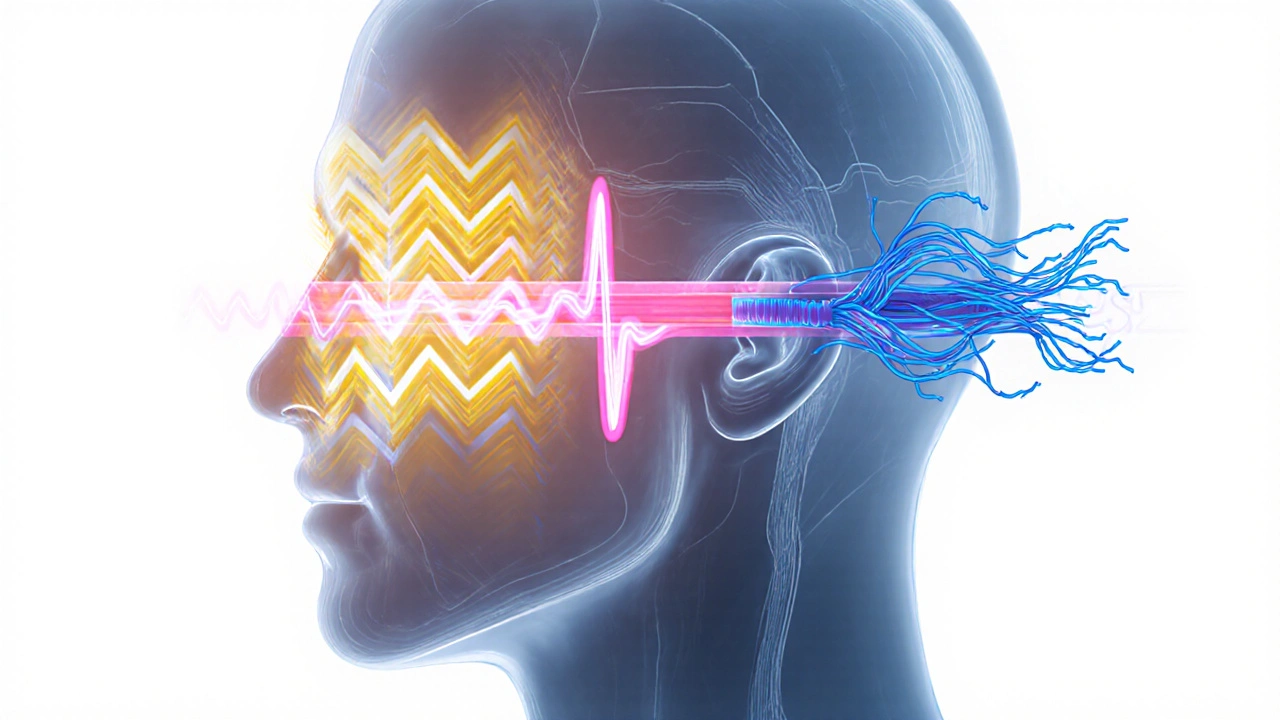
Migraine involves a complex cascade of cortical spreading depression, activation of the trigeminovascular system, and release of vasoactive peptides like CGRP (calcitonin gene‑related peptide). The classic "vascular theory"-that dilated blood vessels cause pain-has been refined; now we know the pain originates from nerve activation, with vessels playing a modulatory role.
Tension‑type headache is primarily a musculoskeletal phenomenon. Prolonged contraction of the occipitofrontalis, trapezius, and sternocleidomastoid muscles leads to peripheral nociceptor sensitization, which can radiate pain to the scalp. Central sensitization may develop in chronic cases, blurring the line between tension headaches and migraine.
Effective Treatment Options
While both headache types benefit from lifestyle tweaks, medication choices differ sharply.
Acute Migraine Relief
- Triptans (e.g., sumatriptan, rizatriptan): serotonin‑1B/1D agonists that abort the trigeminovascular cascade.
- NSAIDs (ibuprofen, naproxen) for mild‑to‑moderate attacks.
- Anti‑nausea agents (metoclopramide) when vomiting is present.
- Emerging CGRP monoclonal antibodies (erenumab) for rapid onset in some patients.
Acute Tension‑type Headache Relief
- Over‑the‑counter NSAIDs (ibuprofen 400mg, aspirin) or acetaminophen.
- Topical muscle rubs containing menthol or capsaicin.
- Brief muscle‑relaxation stretches and massage.
Preventive Strategies
| Migraine | Tension‑type |
|---|---|
| Maintain a consistent sleep schedule; avoid known dietary triggers. | Ergonomic workstation setup; regular posture breaks. |
| Daily magnesium (400mg) or riboflavin (400mg) supplementation. | Stress‑management practices: mindfulness, deep‑breathing, progressive muscle relaxation. |
| Prophylactic meds (beta‑blockers, amitriptyline) for frequent attacks. | Physical therapy focused on neck and shoulder musculature. |
| Track attacks with a headache diary to identify subtle triggers. | Hydration and regular aerobic exercise to reduce overall muscle tension. |

When to Seek Professional Help
Both conditions are usually benign, but red‑flag symptoms warrant immediate evaluation:
- Sudden, "thunderclap" headache reaching maximal intensity in seconds.
- New onset after age 50, especially with hypertension or anticoagulant use.
- Neurological deficits: weakness, vision loss, speech problems.
- Headache that wakes you from sleep repeatedly.
- Headache that worsens despite optimal over‑the‑counter treatment.
Neurologists, headache specialists, and primary‑care physicians can order imaging (MRI, CT) or recommend specialized therapies like nerve blocks.
Practical Self‑Management Checklist
- Identify your pattern: keep a simple log noting pain location, intensity, duration, and any preceding events.
- Match symptoms to migraine vs. tension profiles using the side‑by‑side comparison above.
- Apply the appropriate acute medication within the first hour of onset.
- Implement at least two preventive habits daily (e.g., ergonomic desk setup, magnesium supplement).
- Reassess after four weeks; if attacks persist, schedule a medical review.
Frequently Asked Questions
Can a migraine turn into a tension‑type headache?
It’s possible for a person to experience both conditions, but one doesn’t morph into the other. Migraines involve neurovascular processes, while tension headaches stem from muscle tension. Some sufferers develop a mixed picture, especially when chronic migraine leads to persistent neck strain.
Are over‑the‑counter meds safe for daily use?
Occasional use is fine, but daily NSAID consumption can irritate the stomach lining and raise cardiovascular risk. If you need medication most days, discuss a preventive plan with your doctor rather than relying on continuous OTC dosing.
What lifestyle changes help both migraine and tension headaches?
Regular sleep, staying hydrated, moderate aerobic exercise, and stress‑reduction techniques (meditation, yoga) benefit both. Maintaining a balanced diet and avoiding excessive caffeine also reduces overall headache frequency.
Is caffeine a trigger or a treatment?
In small amounts, caffeine can boost the effectiveness of NSAIDs and even abort a migraine early. However, regular high‑dose intake creates dependence; withdrawal can trigger rebound headaches. Aim for no more than 200mg per day and avoid it during migraine‑prone periods.
Do hormonal birth control methods affect migraines?
Estrogen‑containing contraceptives can increase migraine frequency, especially with aura. Progestin‑only pills or non‑hormonal methods are often better options for migraine sufferers. Always discuss with a healthcare provider before switching.
Understanding the nuances between migraines and tension‑type headaches empowers you to choose the right treatment, avoid common pitfalls, and ultimately reclaim a headache‑free life.

Shriniwas Kumar
October 7, 2025 AT 14:28From a neurovascular standpoint, migraine manifests as a cortical spreading depression followed by trigeminovascular activation, culminating in the release of CGRP and other vasoactive peptides, which in turn sensitize peripheral nociceptors. The ensuing neurogenic inflammation accounts for the photophobia and phonophobia often reported. In contrast, tension-type headache principally involves myofascial trigger points within the occipitofrontalis and trapezius muscles, leading to peripheral nociceptive input without the central neurovascular cascade.
Jennifer Haupt
October 7, 2025 AT 14:30While the article delineates the clinical features adeptly, it is equally vital to recognize the psychosocial dimension: chronic headache sufferers frequently experience diminished quality of life, heightened anxiety, and even depressive symptomatology. A holistic management plan should therefore incorporate cognitive‑behavioral strategies alongside pharmacologic therapy, fostering resilience and empowering patients to regain agency over their health.
NANDKUMAR Kamble
October 7, 2025 AT 14:31One cannot overlook the covert influence of pharmaceutical conglomerates that market triptans as miracle cures while downplaying the long‑term vascular risks. Their funding streams subtly shape research agendas, resulting in an evidence base that favours medication over lifestyle modification.
namrata srivastava
October 7, 2025 AT 14:33The ontological distinction between a migraine and a tension‑type headache resides not merely in symptomatology but in the epistemological frameworks we employ: the former is a manifestation of central sensitization, the latter a peripheral musculoskeletal phenomenon. Appreciating this dichotomy elevates clinical reasoning beyond mere symptom cataloguing.
Priyanka arya
October 7, 2025 AT 14:35👀 Did you know some "miracle" headache pills are actually laced with micro‑doses of substances that keep you hooked? 🤔 Stay vigilant, stay healthy! 🌿✨
Loren Kleinman
October 7, 2025 AT 14:36Understanding the subtle nuances between migraine and tension‑type headache can feel like navigating a labyrinth, but breaking it down step by step makes it manageable. First, consider the quality of pain: migraines are typically throbbing and unilateral, whereas tension headaches present as a steady, bilateral pressure. Second, ask yourself whether you experience associated symptoms such as nausea, visual aura, or heightened sensitivity to light and sound; these are hallmarks of migraine. Third, reflect on your recent lifestyle factors – irregular sleep, stress, and posture can all sway the balance toward tension-type pain. Fourth, keep a simple diary noting the time of onset, duration, and any potential triggers; patterns often emerge after a week or two of diligent recording. Fifth, evaluate your response to over‑the‑counter analgesics; NSAIDs frequently relieve tension headaches but may provide only modest relief for migraines without adjunctive therapy. Sixth, explore prophylactic measures: magnesium supplementation, consistent sleep hygiene, and stress‑reduction practices like mindfulness can reduce migraine frequency. Seventh, consider ergonomic adjustments at your workstation – a properly aligned monitor and supportive chair can alleviate muscular strain that fuels tension headaches. Eighth, stay hydrated; dehydration can exacerbate both conditions but is especially implicated in muscle tension. Ninth, if visual aura or neurological symptoms appear, seek professional evaluation promptly to rule out secondary causes. Tenth, remember that chronic use of NSAIDs carries gastrointestinal and cardiovascular risks, so discuss long‑term strategies with a healthcare provider. Eleventh, biological therapies targeting CGRP signaling have emerged as effective migraine preventatives for refractory cases. Twelfth, regular aerobic exercise has been shown to modulate pain pathways and improve overall vascular health, benefiting both headache types. Thirteenth, avoid excessive caffeine, which can act as a double‑edged sword – helpful in small doses but a trigger when overused. Fourteenth, maintain a balanced diet rich in omega‑3 fatty acids, as inflammation modulation can influence headache propensity. Finally, cultivate patience; finding the optimal combination of lifestyle tweaks and medication often requires iterative trial and error, but the payoff is a life with fewer disruptive headaches.
Sabrina Goethals
October 7, 2025 AT 14:38Wow!! This article is super helpful!!! I love the clear table comparisons!! It's nice to see both the migraine triggers and the tension‑type ones side by side. Definitely going to try the headache diary thing. Thanks a lot!!!
Sudha Srinivasan
October 7, 2025 AT 14:40Stop ignoring the sleep factor; it matters.
Jenny Spurllock
October 7, 2025 AT 14:41It may be useful to cross‑reference the symptom checklist with a weekly stress inventory; many people discover that their tension headaches correlate with days they report high work‑related anxiety.
Bart Cheever
October 7, 2025 AT 14:43The article is fine but the language is too flowery; plain language works better for most folks.
Maude Rosièere Laqueille
October 7, 2025 AT 14:45Practical tip: keep a small notebook on your nightstand to jot down any headache occurrences as soon as you wake up. Over time, you’ll notice trends that can guide both acute and preventive strategies, especially when paired with the lifestyle modifications outlined above.
Amanda Joseph
October 7, 2025 AT 14:46Great, another “quick guide” that pretends to replace a doctor’s advice. 🙄
Kevin Aniston
October 7, 2025 AT 14:48Really appreciate the thoroughness of the earlier post – it gave me a solid framework for dissecting my own symptoms. Building on that, I’d add that consistency in your preventive routine is just as crucial as the components themselves. For instance, magnesium supplements only work if you take them daily, not sporadically when a headache looms. Similarly, a relaxation exercise practiced for five minutes each morning yields far better outcomes than a 30‑minute session once a month. Another point worth highlighting is that many patients overlook the role of vestibular therapy; if you experience vertigo alongside migraine aura, incorporating balance training can mitigate that component. Finally, don’t be afraid to experiment under medical supervision – sometimes a low‑dose beta‑blocker combined with a dietary tweak can transform a chronic migraine pattern into a manageable occasional occurrence.
kiran kumar
October 7, 2025 AT 14:50Honestly i think all these guidelines are overcomplicated. just lay down and take a nap, that works everytime.
Brian Johnson
October 7, 2025 AT 14:51I hear you – the journey through chronic pain can feel isolating, but remember that sharing your experiences, even in brief snippets, builds a supportive community that reinforces coping strategies and offers fresh perspectives.
Jessica Haggard
October 7, 2025 AT 14:53What a comprehensive breakdown! For anyone juggling a multicultural lifestyle, remember to consider dietary triggers specific to your heritage – certain spices, fermented foods, or regional cough syrups can sneakily act as migraine provocateurs.