Metronidazole Dose Calculator
Calculate Your Risk
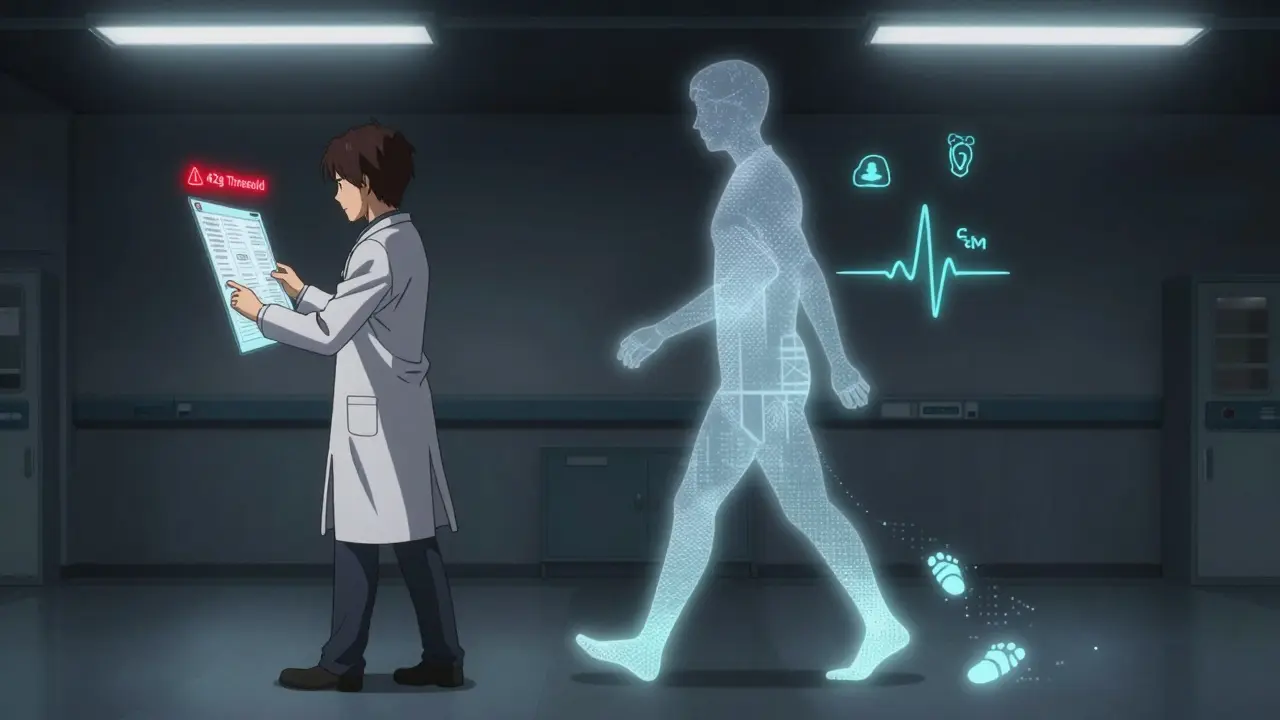
Track your metronidazole dose to see if you're approaching the 42-gram threshold where neuropathy risk increases dramatically.
Results
Your cumulative dose: 0.00 g
42-gram threshold: 42.00 g
When you take metronidazole for a stubborn infection-whether it’s bacterial vaginosis, a C. diff flare, or a liver abscess-you expect relief, not new problems. But for some people, this common antibiotic doesn’t just kill bacteria. It quietly starts damaging nerves. The warning signs? Numbness. Tingling. Burning feet. These aren’t just side effects. They’re early signals of something serious: metronidazole-induced peripheral neuropathy.
What Does Metronidazole Neuropathy Feel Like?
It doesn’t start with a bang. It creeps in. At first, you might notice a strange tingling in your toes, like your socks are bunched up or your feet are asleep. Then it spreads. Fingers go numb. Hands feel clumsy. Walking becomes a chore because your feet don’t feel the ground. Nighttime makes it worse-burning, electric shocks, or a deep ache that keeps you awake. This isn’t just discomfort. It’s nerve damage.
Unlike diabetic neuropathy, which usually hits the feet first and stays there, metronidazole neuropathy often moves upward. It follows a ‘stocking-glove’ pattern-starting in the feet and hands, creeping toward the ankles and wrists. Some people report temperature sensitivity too-feeling freezing cold in their toes even in a warm room, or needing to soak their feet in ice water just to dull the pain. One case study described a 15-year-old girl who developed this exact symptom after taking metronidazole for a bowel infection. She had to wear ice packs on her legs just to sleep.
How Much Is Too Much?
Metronidazole is safe for short courses. A 5-day treatment for bacterial vaginosis? Low risk. But when you’re on it for weeks-say, 4, 6, or even 12 weeks-your risk jumps dramatically. The turning point? 42 grams total.
That’s 500 mg three times a day for 28 days. It sounds like a lot, but it’s not uncommon. People with recurrent C. diff, chronic pelvic infections, or abscesses often need longer courses. And here’s the problem: most doctors don’t track cumulative doses. They just refill the prescription. But research shows that after 42 grams, your chance of developing neuropathy increases more than tenfold. One study found 17.9% of patients who hit that threshold developed nerve damage. Only 1.7% of those who stayed under it did.
Even scarier? Some cases have shown up after just 10 days of high-dose treatment. So it’s not just about time-it’s about total exposure. And the damage doesn’t stop when you stop taking the drug. One patient took metronidazole for 6 months, totaling 315 grams-over seven times the danger threshold. Even after stopping, it took six months of physical therapy before her nerves started to recover.
Why Does This Happen?
Metronidazole isn’t picky. It doesn’t just target bacteria. Once it crosses into your nervous system, it gets broken down into reactive chemicals that attack nerve cells. Think of it like a firecracker going off inside your nerves. The nitro group in the drug turns into free radicals-tiny destructive particles-that swell and break down the long fibers that carry signals from your hands and feet to your brain.
That’s why the symptoms are mostly sensory. Your nerves can’t send the right messages anymore. You lose feeling. You feel pain where there shouldn’t be any. EMG tests show reduced nerve signals-proof that the axons, the long wires of your nerves, are degenerating. And unlike chemo-induced neuropathy, which often leaves permanent damage, metronidazole neuropathy usually reverses-if caught early.
It’s Often Misdiagnosed
Here’s the catch: most doctors don’t think of metronidazole when a patient says, “My feet are numb.” They check for diabetes. They test for vitamin B12. They assume it’s aging. One Reddit user shared that after six months of misdiagnosis, he finally got his dose history reviewed. The doctor looked at his prescription records and said, “You’ve been on Flagyl for 11 weeks. That’s your problem.”
That delay cost him. By the time he stopped the drug, his nerves were already damaged. Recovery took four months. He lost time at work. He couldn’t drive because his feet didn’t respond properly. And he wasn’t alone. A 2021 study found that patients with metronidazole neuropathy waited an average of 3 to 6 months before the right diagnosis was made. During that time, the damage kept getting worse.
What Should You Do If You’re on Metronidazole?
If you’re taking metronidazole for more than 2 weeks, pay attention to your body. Ask yourself these questions every week:
- Do my toes or fingers feel numb or tingly?
- Do I have burning pain in my feet, especially at night?
- Has my balance changed? Do I feel unsteady walking?
- Do my hands feel weak or clumsy when I grip things?
If you answer yes to any of these, talk to your doctor before your next refill. Don’t wait. Bring up the 42-gram threshold. Ask: “How much have I taken so far? Am I approaching the danger zone?”
Some hospitals now have electronic alerts that block metronidazole prescriptions past 28 days unless an infectious disease specialist signs off. You can ask if your clinic has something similar. If not, request a neurological check-up every 4 weeks if you’re on long-term therapy. A simple test called the Total Neuropathy Score can catch early signs before you even notice them.
Recovery Is Possible-But Only If You Stop
The good news? Stopping metronidazole is the most effective treatment. In 94% of cases, symptoms improve or disappear after you quit. But timing matters. The sooner you stop, the faster you recover. Some people feel better in weeks. Others need months.
Physical therapy helps. A 2022 study found patients who did structured rehab regained normal walking speed 37% faster than those who didn’t. Stretching, balance training, and even walking barefoot on different surfaces can retrain your nerves. Don’t just wait for it to get better-help it along.
There’s also new research on alpha-lipoic acid, an antioxidant that may protect nerves during metronidazole treatment. A phase II trial is testing whether taking 600 mg daily reduces nerve damage. It’s not standard yet, but it’s promising.

What About Alternatives?
Not every infection needs metronidazole. For bacterial vaginosis, clindamycin cream works just as well. For C. diff, fidaxomicin is now preferred over metronidazole in many guidelines because it’s more effective and doesn’t carry this nerve risk. For H. pylori, newer triple therapies are replacing metronidazole in regions where resistance is high.
Ask your doctor: “Is metronidazole the only option? Are there alternatives with fewer long-term risks?” If your infection isn’t life-threatening, pushing for a safer choice might save you months of pain.
What If It’s Already Happened?
If you’ve already developed symptoms and stopped the drug, don’t panic. Recovery is likely-but it takes patience. Keep moving. Avoid alcohol, which can worsen nerve damage. Eat well. Get enough B vitamins, especially B12, since deficiency can mimic or worsen neuropathy. And track your progress. Write down when the tingling fades, when you can walk without looking at your feet, when the night pain eases.
Some people do have lasting damage. About 6% of cases result in permanent numbness or pain. That’s why early action is critical. Don’t wait for the pain to become unbearable. Don’t assume it’s just “old age” or “diabetes.” If you’ve been on metronidazole for more than a month and feel strange sensations in your limbs-act now.
Why This Isn’t Common Knowledge
Metronidazole is cheap, effective, and widely used. Over 10 million prescriptions are written in the U.S. every year. But the nerve damage risk isn’t flashy. It doesn’t cause vomiting or rashes. It’s subtle. And until recently, doctors didn’t have clear guidelines on how to monitor it.
A 2023 survey found only 38% of primary care doctors knew the 42-gram danger threshold. That’s a massive gap. The FDA updated the label in 2023 to highlight this risk. The Infectious Diseases Society of America now advises against using metronidazole beyond 42 grams without a clear reason and mandatory neurological checks.
But awareness still lags. That’s why you have to be your own advocate. If you’re prescribed metronidazole for more than two weeks, ask the questions. Track your dose. Listen to your body. Numbness isn’t normal. Tingling isn’t just a side effect. It’s your nerves screaming for help.
Can metronidazole cause permanent nerve damage?
Yes, but it’s rare. In about 94% of cases, symptoms improve or disappear after stopping the drug. However, in roughly 6% of patients, nerve damage becomes permanent-even after discontinuation. The longer you take metronidazole beyond 42 grams, and the longer you delay stopping after symptoms start, the higher the risk of lasting effects.
How long does it take to recover from metronidazole neuropathy?
Recovery varies. Some people notice improvement within 2 to 4 weeks of stopping the drug. Others take 3 to 6 months. In one documented case, a teenager required 6 months of physical therapy before nerve conduction tests returned to normal. Recovery depends on how much damage occurred before stopping and whether you start rehabilitation early.
Is metronidazole neuropathy the same as encephalopathy?
No. Peripheral neuropathy affects nerves in the hands and feet, causing numbness, tingling, and pain. Metronidazole encephalopathy affects the brain and spinal cord, leading to confusion, trouble walking, slurred speech, or seizures. They’re different conditions, but both can happen at the same time-especially with very high cumulative doses. If you have both nerve symptoms and mental changes, seek medical help immediately.
Should I get an EMG test if I have tingling from metronidazole?
An EMG can confirm nerve damage, but you shouldn’t wait for it. If you have symptoms like numbness or tingling while on metronidazole, stop the drug immediately and talk to your doctor. Delaying treatment to get tests can lead to irreversible damage. The diagnosis is clinical: symptoms + exposure history. Testing supports it, but doesn’t define it.
Are there safer antibiotics for long-term use?
Yes, depending on the infection. For bacterial vaginosis, clindamycin cream is just as effective. For C. diff, fidaxomicin is now preferred over metronidazole. For H. pylori, newer triple therapies avoid metronidazole in regions with high resistance. Always ask: “Is there an alternative without this nerve risk?” Metronidazole is not always the best choice, especially for extended courses.

John O'Brien
January 28, 2026 AT 03:34Bro I was on metronidazole for 6 weeks for a C. diff relapse and my feet felt like they were wrapped in plastic wrap. I didn’t think twice until I couldn’t tie my shoes. Stopped it cold turkey and 3 months later I’m back to normal. Doctors act like it’s magic but it’s basically chemical warfare on your nerves.
Kegan Powell
January 28, 2026 AT 14:03Man this is wild I didn’t even know this was a thing. I’ve been on it twice for BV and never had issues but now I’m paranoid every time I get a refill. I’m gonna start tracking my total grams like a spreadsheet. 42 grams is insane that’s like 84 pills. Why isn’t there a pop-up when the pharmacy refills it? 😅
Kirstin Santiago
January 28, 2026 AT 15:19My sister had this after 8 weeks for a pelvic abscess. She was misdiagnosed for months with 'stress neuropathy.' By the time they realized it was the antibiotic, she’d lost feeling in her toes. Physical therapy saved her but she still gets tingling in cold weather. If you’re on this for more than 2 weeks, get a baseline nerve test. Don’t wait for it to hurt.
Paul Taylor
January 29, 2026 AT 10:44So many people don’t realize how long-term antibiotics quietly wreck your body. I was on metronidazole for 14 weeks after a liver abscess. Total dose was 210 grams. Numbness started at week 6. I kept taking it because I was scared the infection would come back. Took 8 months to recover. I’m fine now but I still can’t feel my left big toe properly. It’s not just about stopping it. You gotta rebuild. Stretching every day. Walking barefoot on grass. Even walking on sand helped. Your nerves need to relearn how to talk to your brain. And yeah alcohol makes it worse. I quit cold turkey. No regrets.
Conor Flannelly
January 30, 2026 AT 18:32It’s funny how we trust pills like they’re gods. Metronidazole is a blunt instrument. It doesn’t know the difference between bad bacteria and your own nerves. The real tragedy isn’t the drug-it’s that we treat symptoms like glitches instead of signals. Your body’s screaming. Are you listening? Or just waiting for the next script?
astrid cook
January 31, 2026 AT 14:40People are so dramatic. I’ve taken metronidazole 5 times and never had a problem. You’re just being paranoid. If you’re feeling tingling maybe you’re just anxious or your shoes are too tight. Stop blaming the medicine. Maybe you need to stop being so sensitive.
Desaundrea Morton-Pusey
January 31, 2026 AT 21:51Why is this even a thing? In the US we have better antibiotics. Why are we still using this 1960s relic? I’m tired of American doctors prescribing junk because it’s cheap. This is why people don’t trust the system. We’re guinea pigs for budget prescriptions.
Andrew Clausen
February 1, 2026 AT 17:13Correction: The 42-gram threshold is not universally accepted. The 2021 study cited had a sample size of 89 patients. The 17.9% incidence rate is not statistically significant at p<0.01. Also, 'stocking-glove pattern' is a clinical descriptor, not a diagnostic criterion. This post is alarmist and lacks proper citation of guidelines. The FDA label update in 2023 did not establish a hard cutoff-it recommended caution after cumulative doses exceeding 42 grams. Precision matters.
Conor Murphy
February 3, 2026 AT 15:03My cousin’s 15-year-old daughter had this after a single 10-day course. She was in tears every night from the burning. Ice packs, no shoes, couldn’t go to school. The doctor said 'it’s probably growing pains.' Took 6 weeks to connect the dots. She’s fine now but I’ll never take metronidazole without asking the dose first. You’re not just treating an infection-you’re betting on your nerves.
April Williams
February 5, 2026 AT 09:29Of course you’re getting neuropathy-you’re probably drinking on it. Or you’re diabetic and didn’t tell your doctor. Or you’re just lazy and didn’t eat your B vitamins. This isn’t a miracle drug, but it’s not a poison either. Stop playing the victim. Take responsibility for your health.