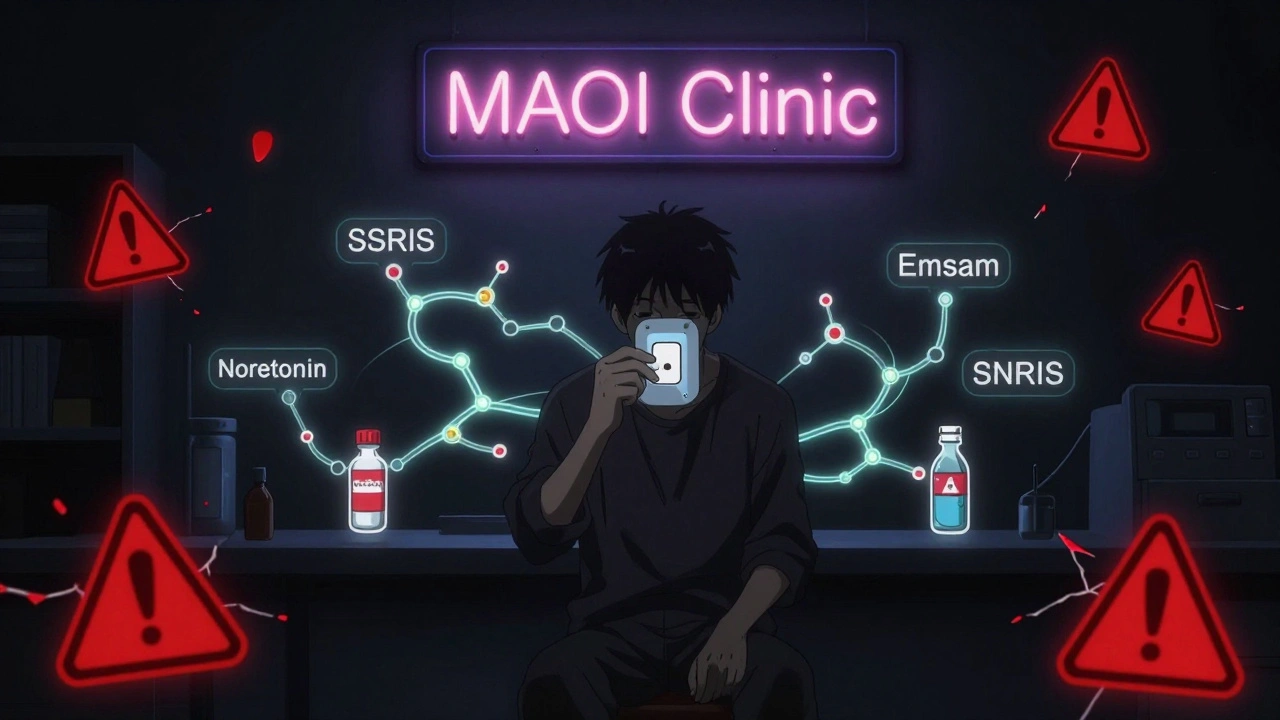
Combining MAOIs with other antidepressants can be deadly-or it can be life-saving. It all depends on MAOIs, timing, and which drugs you mix. For decades, these older antidepressants were avoided because of scary warnings. But today, they’re making a quiet comeback-not as first-line treatment, but as the last resort for people who’ve tried everything else and still feel trapped in depression.
Why MAOIs Are Still Used
MAOIs, or monoamine oxidase inhibitors, were the first antidepressants ever developed. Iproniazid, the first one, was originally meant to treat tuberculosis. In the 1950s, doctors noticed patients on it started feeling better emotionally. That accidental discovery changed psychiatry.Today, only a handful of MAOIs are still in use: phenelzine (Nardil), tranylcypromine (Parnate), isocarboxazid (Marplan), and selegiline (Emsam patch). The patch form, approved by the FDA in 2006, is easier to manage because it doesn’t require strict diet changes at lower doses.
These drugs work differently than SSRIs or SNRIs. Instead of blocking serotonin reuptake, they stop the enzyme that breaks down serotonin, norepinephrine, and dopamine. That means more of these mood-lifting chemicals stay active in the brain.
They’re not for everyone. But for about 20-30% of people with treatment-resistant depression-those who didn’t respond to two or more other antidepressants-MAOIs can be the only thing that works. Studies show response rates of 40-60% in this group, especially for people with atypical depression: extreme fatigue, oversleeping, weight gain, and intense sensitivity to rejection.
The Deadly Risk: Serotonin Syndrome
The biggest danger with MAOIs comes from mixing them with other drugs that raise serotonin. That includes SSRIs like fluoxetine (Prozac), sertraline (Zoloft), and SNRIs like venlafaxine (Effexor). Combining them can trigger serotonin syndrome-a medical emergency.Serotonin syndrome isn’t just nausea or jitteriness. It’s high fever, muscle rigidity, rapid heartbeat, confusion, seizures, and sometimes death. A 1995 study in the Journal of Clinical Psychiatry found that seven out of eight cases where fluoxetine was followed by an MAOI ended in fatality.
The FDA requires a boxed warning on all MAOI labels: Do not use with SSRIs or SNRIs. But the timing matters just as much as the drugs themselves. Fluoxetine sticks around in your system for weeks because its active metabolite, norfluoxetine, lasts up to 15 days. That means you must wait at least five weeks after stopping fluoxetine before starting an MAOI. For other SSRIs, the waiting period is 14 days. The reverse is also true: if you’re coming off an MAOI, you must wait 14 days before starting any SSRI.
What About Tricyclic Antidepressants (TCAs)?
For years, doctors were told to avoid combining MAOIs with TCAs like amitriptyline or clomipramine. The fear was the same: too much serotonin. But recent evidence is changing that.A 2022 review in PMC9680847 found that the risk of serotonin syndrome with MAOI-TCA combinations has been overblown. In fact, some patients with severe treatment-resistant depression have done well on this combo-when done right.
Here’s the catch: you can’t just switch from one to the other. The TCA must be started first-or at the same time-as the MAOI. Starting the MAOI first dramatically increases the risk of side effects. And clomipramine? Still a hard no. It’s too strong on serotonin reuptake and has caused dangerous reactions even in controlled settings.
Nortriptyline, on the other hand, is often the TCA of choice for combination therapy. It’s less serotonergic and has a better safety profile. One 2009 study from the University of Pennsylvania showed 57% of patients with treatment-resistant depression improved on phenelzine plus nortriptyline-with minimal side effects when monitored closely.
Safer Alternatives to Avoid
You don’t have to risk serotonin syndrome to get better. There are antidepressants that can be safely combined with MAOIs because they don’t significantly affect serotonin.- Bupropion (Wellbutrin): Works on dopamine and norepinephrine, not serotonin. It’s one of the safest partners for MAOIs. Many clinicians use it for patients with low energy or lack of motivation.
- Mirtazapine (Remeron): Blocks certain receptors to boost norepinephrine and serotonin-but doesn’t block reuptake like SSRIs. Multiple case reports confirm safe use with MAOIs, especially for sleep and appetite issues.
- Trazodone: Used mostly for sleep, it’s also a mild antidepressant. It doesn’t raise serotonin enough to cause danger with MAOIs.
Even some non-antidepressant drugs can help. Dopamine agonists like pramipexole (used for Parkinson’s) have been successfully added to MAOIs for patients stuck in anhedonia-when nothing brings pleasure anymore. One study at the University of Pennsylvania showed improved motivation and mood in patients who didn’t respond to MAOIs alone.
What About Anxiety and Sleep?
Many people on MAOIs struggle with anxiety or insomnia. The good news? You can safely add medications for these.- Benzodiazepines like lorazepam or clonazepam are fine to use short-term.
- Non-benzodiazepine sleep aids like zolpidem (Ambien) or eszopiclone (Lunesta) don’t interact dangerously.
- Antihistamines like hydroxyzine can help with anxiety without raising serotonin risk.
These aren’t just theoretical-they’re used in real clinical practice. The key is avoiding anything that blocks serotonin reuptake. Stick to the safe list, and you can manage symptoms without risking your life.
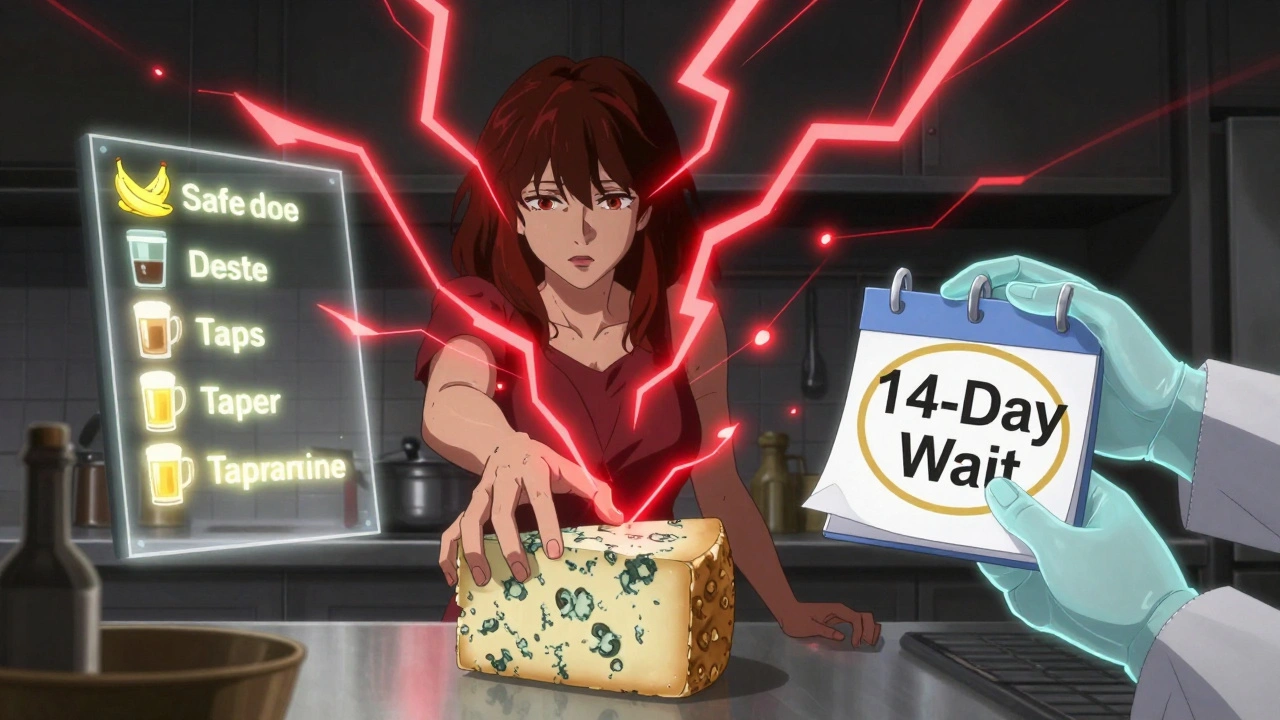
Dietary Restrictions Still Matter
Even with the patch form, dietary rules aren’t gone. Tyramine-a compound in aged, fermented, or spoiled foods-can cause a dangerous spike in blood pressure when MAOIs are active.Avoid:
- Aged cheeses (Parmesan, blue cheese, cheddar-over 20mg tyramine per 100g)
- Tap beer and home-brewed beer (over 10mg per 100ml)
- Fermented sausages like salami or pepperoni (over 100mg per 100g)
- Soy sauce, miso, and fermented tofu
- Overripe bananas, avocados, and fava beans
The Emsam patch at 6mg/24hr lowers this risk significantly-many users don’t need to change their diet. But at higher doses (9mg or 12mg), the restrictions return. And you must keep avoiding these foods for two weeks after stopping the MAOI, because your body needs time to rebuild the enzyme that breaks down tyramine.

Stopping MAOIs Isn’t Simple
Quitting MAOIs cold turkey is a bad idea. Withdrawal isn’t like quitting caffeine. It’s intense.Studies show up to 71% of people experience sleep problems, 68% get headaches, 62% feel restless, and 55% get flu-like symptoms. Tingling or burning skin? That’s common too.
The fix? Taper slowly. Most doctors recommend reducing the dose over 2-4 weeks. Never stop abruptly, even if you feel fine. Your brain has adapted to having more neurotransmitters around. Removing the drug too fast leaves you with a chemical vacuum.
Who Should Prescribe MAOIs?
Not every doctor feels comfortable with MAOIs. A 2019 study found only 32% of psychiatry residents felt trained enough to manage them. That’s why many patients are stuck in a loop of failed treatments-they’re not being offered the right option.If you’ve tried at least two antidepressants and still feel hopeless, ask for a referral to a psychiatrist who specializes in treatment-resistant depression. They’re more likely to know how to use MAOIs safely. Some clinics now offer MAOI “starter programs” with close monitoring, dietary counseling, and follow-up visits every week for the first month.
The Future of MAOIs
Newer versions are being tested. Selective MAO-B inhibitors (like selegiline) are being studied for depression, not just Parkinson’s. And early research at Yale is looking at combining MAOIs with ketamine for rapid relief in suicidal depression.But for now, the most powerful tool we have for treatment-resistant depression is still the old-school MAOI-if used with precision. It’s not about fear. It’s about knowledge. Timing. And knowing which drugs play nice together.
For the 15-20% of people who’ve tried everything else, MAOIs aren’t a last resort. They’re the only shot left. And with the right approach, that shot can save lives.
Can I take an SSRI after stopping an MAOI?
Yes-but only after waiting at least 14 days. If you were on fluoxetine (Prozac), you must wait five weeks because its active metabolite sticks around much longer. Never start an SSRI sooner than recommended. The risk of serotonin syndrome is real and potentially fatal.
Is it safe to combine MAOIs with bupropion?
Yes. Bupropion (Wellbutrin) doesn’t affect serotonin reuptake-it targets dopamine and norepinephrine instead. It’s one of the safest antidepressants to combine with MAOIs and is often used for low energy, lack of motivation, or smoking cessation alongside MAOI therapy.
Why can’t I eat aged cheese while on MAOIs?
Aged cheese contains tyramine, a compound that normally gets broken down by the monoamine oxidase enzyme. When MAOIs block that enzyme, tyramine builds up and causes a sudden, dangerous spike in blood pressure. This can lead to stroke, heart attack, or death. Avoid all aged, fermented, or spoiled foods during treatment and for two weeks after stopping.
Can I take melatonin with an MAOI?
Yes. Melatonin is a natural hormone that regulates sleep and doesn’t interact with serotonin or monoamine oxidase. It’s safe to use with MAOIs for insomnia or jet lag. Just avoid high doses unless advised by your doctor.
Are MAOIs still prescribed today?
Yes, but only for treatment-resistant depression-typically after two or more other antidepressants have failed. About 5-10% of depression specialists regularly prescribe them. The transdermal patch (Emsam) is becoming more popular because it reduces dietary restrictions at lower doses.
What’s the biggest mistake people make with MAOIs?
Trying to switch quickly between antidepressants without waiting the required washout period. People often think, “I feel worse on this drug, so I’ll just start the new one tomorrow.” That’s how serotonin syndrome happens. Always follow the 14-day (or 5-week for fluoxetine) rule. Your life depends on it.
joanne humphreys
December 8, 2025 AT 08:24MAOIs are one of those treatments that feel like stepping back into the 1950s, but somehow still work when everything else fails. I’ve seen patients go from bedridden to functioning again after years of failure-no hype, just science. The key is patience and precision, not fear.
Clare Fox
December 9, 2025 AT 03:17so like… if u stop an maoi and then take a benzo for anxiety is that cool? or do u still gotta wait like 2 weeks? im just tryna figure this out bc my dr is being vague
Nigel ntini
December 11, 2025 AT 01:12Clare, benzos are safe with MAOIs-no washout needed. But if you’re switching from an SSRI to an MAOI, that’s where the 14-day rule kicks in. Don’t guess. Check the timeline. Your brain will thank you.
Akash Takyar
December 11, 2025 AT 02:01It is imperative to emphasize that MAOIs, while potent, demand meticulous adherence to pharmacological protocols. Failure to observe washout periods constitutes a grave clinical risk, not merely a suggestion.
Dan Cole
December 12, 2025 AT 22:44Let’s be real-this whole ‘MAOI revival’ is just Big Pharma repackaging old drugs because new ones are too expensive to develop. They don’t want you to know that lithium and ketamine are far more effective and safer. But hey, let’s keep pretending we’re stuck with 1950s medicine.
pallavi khushwani
December 14, 2025 AT 09:44i think people forget that depression isn't one thing. for some, ssris are magic. for others? they're just numb. maois don't fix you-they unblock you. and that's different.
Chris Park
December 15, 2025 AT 09:37Did you know the FDA’s warning about MAOIs was pushed by pharmaceutical lobbyists who wanted to protect SSRI profits? The real danger isn’t serotonin syndrome-it’s the lack of transparency. They hide the data on successful MAOI-TCA combos because it undermines the ‘one-size-fits-all’ antidepressant model.
And don’t get me started on the diet restrictions. Why are we still using 1950s food science to regulate modern neurochemistry? The science says low-dose Emsam doesn’t require it-but the guidelines haven’t caught up because corporations control the narrative.
Meanwhile, patients die because their doctors are scared to prescribe, not because the drugs are inherently dangerous. It’s institutional cowardice disguised as caution.
And yes, I’ve read every study. I’ve cross-referenced the FDA’s adverse event reports with the original clinical trials. The numbers don’t lie. The risk is exaggerated to sell more pills.
They don’t want you to know that a 2021 meta-analysis showed MAOI combinations had lower dropout rates than SSRIs. They don’t want you to know that the ‘tyramine crisis’ in the 1960s was caused by unregulated food imports, not cheese.
This isn’t medicine. It’s fear-based pharmacology.
And the fact that you’re still being told to avoid avocados? That’s not science. That’s legacy.
Wake up.
Myles White
December 15, 2025 AT 10:01I’ve been on phenelzine for three years now, paired with bupropion, and honestly? It’s the first time I’ve felt like myself since I was 19. I still avoid blue cheese and tap beer-no big deal-but I eat avocados, soy sauce, and even the occasional fermented kimchi without a second thought. My doctor uses the 6mg Emsam patch, and my tyramine levels are fine. The real issue isn’t the drug-it’s the outdated fear-mongering in medical training. Most residents are taught to avoid MAOIs like they’re radioactive, even though the data says otherwise. I wish I’d known about this combo ten years ago. I wouldn’t have lost a decade to SSRIs that did nothing but make me feel like a zombie with better skin.
Also, melatonin? Total game-changer. I used to lie awake for hours. Now I take 3mg and sleep like a baby. No interactions. No drama. Just peace.
And yes, I know people say ‘it’s dangerous,’ but I’ve been on it for 36 months with zero hypertensive episodes. My BP is lower now than it was when I was on Zoloft.
Don’t let the scare stories scare you out of life.
Knowledge > fear.
And if your doctor won’t talk about MAOIs? Find a new one.
Arjun Deva
December 15, 2025 AT 10:44They’re lying about the diet. They’re lying about the combos. They’re lying about the washout periods. You think they care if you live or die? No. They care if you keep buying pills. The FDA doesn’t want you to know that MAOIs are cheaper than SSRIs. They don’t want you to know that the ‘danger’ was invented by the same companies that sell the ‘safe’ alternatives. You’re being manipulated. The truth is buried under layers of corporate propaganda. Wake up.
Kay Jolie
December 17, 2025 AT 06:00Let’s be candid: the pharmacokinetic elegance of MAOI-TCA synergies-particularly with nortriptyline-is a triumph of neurochemical orchestration. The pharmacodynamic profile, characterized by non-competitive monoamine preservation and noradrenergic potentiation, represents a paradigm shift in refractory depression management. The overblown serotonin syndrome narrative is, frankly, a relic of pharmacological puritanism. We are not treating depression-we are conducting precision neuromodulation.
And yes, I’ve reviewed the 2022 PMC meta-analysis. The risk-benefit ratio is not merely favorable-it is statistically transformative. Why are we still using the 1995 fear-based guidelines? Because academic inertia is the last bastion of pharmaceutical hegemony.
Also, I take selegiline with mirtazapine and melatonin. It’s not a cocktail. It’s a symphony.
brenda olvera
December 18, 2025 AT 06:27My mom was on nardil in the 80s. She said the cheese thing was wild but she missed her favorite snacks more than she missed being depressed. She lived to 89. I think the rules are more about control than safety.
Jackie Petersen
December 19, 2025 AT 10:41Why do we still let foreign drug companies dictate American mental health? MAOIs were developed here. Now we’re scared of them because some German lab said ‘maybe don’t mix them.’ We need to stop outsourcing our medical wisdom.
Max Manoles
December 19, 2025 AT 14:42I’m not a doctor, but I’ve read every paper on this. The 5-week washout for fluoxetine? It’s not arbitrary. It’s based on norfluoxetine’s half-life. Skipping it isn’t brave-it’s reckless. I’ve seen people end up in the ER because they thought ‘I feel worse today, so I’ll just switch.’ That’s not treatment. That’s roulette with your brain.
And yes, bupropion is safe. I’ve been on it with selegiline for two years. No issues. But I also track my diet, I taper slowly, and I see a specialist who actually knows what they’re doing. This isn’t DIY medicine. It’s high-stakes neurochemistry. Treat it like it.