Kaposi Sarcoma & Sexual Health: Relationship Guide
Kaposi Sarcoma (KS) itself is not sexually transmitted. However, the virus that causes it, HHV-8, can spread through:
- Saliva
- Blood
- Sexual fluids
Most people infected with HHV-8 never develop KS unless their immune system is compromised.
When talking to your partner about KS, consider these steps:
- Pick a quiet, private moment
- Use plain language to explain the condition
- Clarify that KS lesions aren't contagious
- Share your treatment plan (like ART)
- Encourage questions and honest discussion
To maintain intimacy safely:
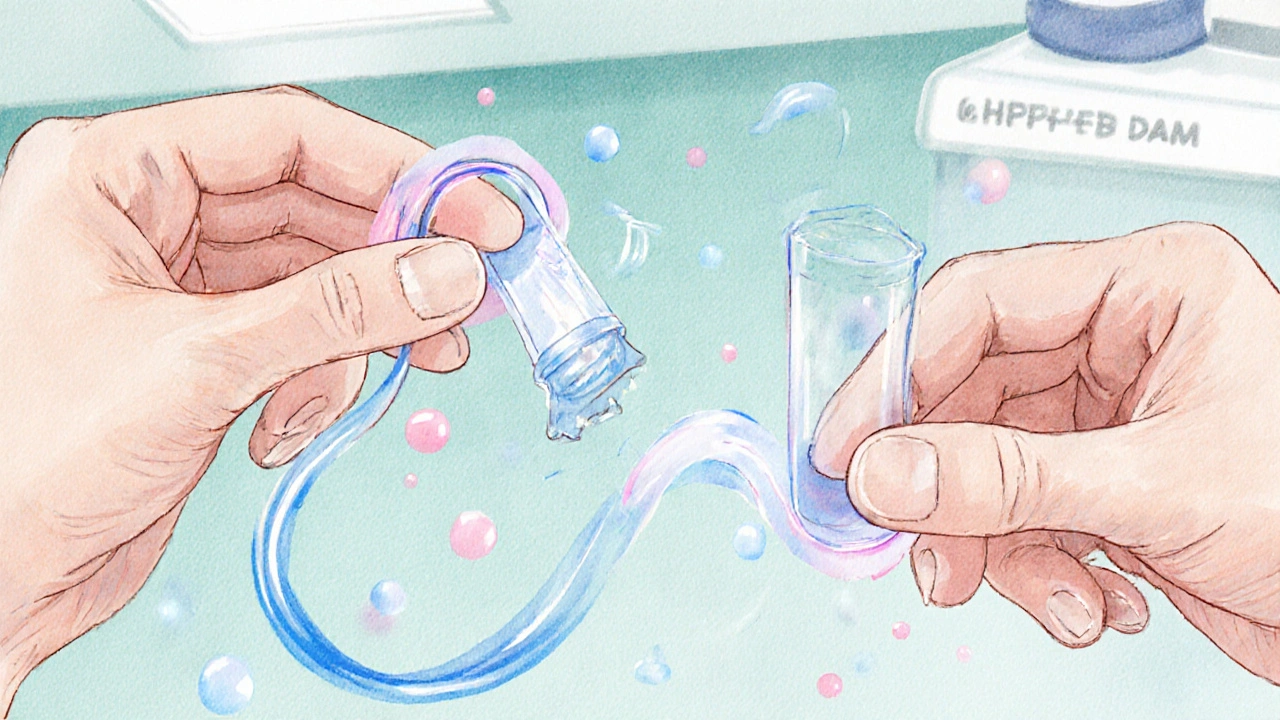
- Use condoms during sexual activity
- Use dental dams for oral-genital contact
- Avoid direct contact with active lesions
- Keep wounds clean and treated
- Stay on effective ART to lower viral load
These steps help protect both partners while preserving intimacy.
Managing the emotional aspects of KS:
- Normalize the experience with others facing similar challenges
- Consider couples counseling focused on chronic illness
- Join support groups for people with KS or HIV
- Explore non-sexual forms of intimacy
- Celebrate small victories and milestones
Test your understanding of Kaposi Sarcoma and its impact on sexual health.
Quiz Results
Quick Takeaways
- Kaposi Sarcoma (KS) is caused by HHV‑8 and often shows up in people with weakened immunity, especially HIV‑positive individuals.
- KS itself is not sexually transmitted, but the virus that causes it (HHV‑8) can spread through saliva, blood, and sexual fluids.
- Open communication, safe‑sex practices, and regular medical follow‑up keep intimacy safe and enjoyable.
- Emotional support - from counselors, support groups, or trusted friends - helps manage anxiety and stigma.
- Know the signs of active lesions and when to pause certain activities to protect both partners.
When a diagnosis of Kaposi Sarcoma a cancer linked to human herpesvirus8 that often appears in people with weakened immune systems lands, questions about love, sex, and intimacy surface quickly. You might wonder if you can be physically close, whether your partner is at risk, or how to talk about new limitations. This guide walks you through the medical facts, practical tips, and emotional tools you need to keep relationships thriving while managing KS.
What Exactly Is Kaposi Sarcoma and How Does It Relate to Sexual Health?
KS is a vascular tumor that manifests as purple‑red or brown patches on the skin, mouth, or internal organs. The root cause is human herpesvirus8 often abbreviated HHV‑8, a member of the herpesvirus family. While HHV‑8 can be spread through sexual contact, most people who contract it never develop KS unless their immune system is compromised.
In practice, the strongest link is between KS and HIV/AIDS a condition that lowers CD4 counts and weakens immune response. Effective antiretroviral therapy (ART) medication regimens that suppress HIV replication and restore immune function can reduce the risk of KS flare‑ups and shrink existing lesions.
Understanding these relationships clears up a common myth: KS itself does not travel through sexual fluids. What can be transmitted is HHV‑8, and only when there’s direct contact with infected saliva or blood, which is why safe‑sex habits still matter.
Talking to Your Partner: Building Trust and Clarity
Starting a conversation about KS can feel intimidating, but honesty breeds confidence. Here’s a simple roadmap:
- Pick the right moment. Choose a quiet, private setting where you won’t be rushed.
- Explain the basics. Use plain language - “I have a skin condition caused by a virus that usually shows up when the immune system is low.”
- Address transmission myths. Reassure them that KS itself isn’t contagious, but HHV‑8 can be spread through saliva or blood.
- Share your health plan. Let them know you’re on ART, you have regular check‑ups, and you monitor your CD4 count a lab measure of immune strength.
- Invite questions. Give space for their concerns and answer honestly, or offer to look up answers together.
Couples who practice open dialogue report less anxiety and more satisfaction in the bedroom, even when medical challenges arise.
Safe Intimacy: Practical Tips for Sexual Activity
Safety isn’t about abstaining; it’s about smart choices that protect both partners while keeping pleasure on the table.
- Condoms are still key. They block blood and seminal fluid, reducing HHV‑8 exposure.
- Consider dental dams. For oral‑genital contact, a thin latex barrier prevents saliva exchange.
- Watch lesion locations. If KS patches cover the genitals or oral cavity, avoid direct contact until a doctor clears them or they have healed.
- Maintain good wound care. Keep any sores clean; infection can increase viral shedding.
- Stay on treatment. Consistent ART lowers viral load, which indirectly reduces HHV‑8 activity.
These steps create a safety net without turning intimacy into a chore.
Emotional Wellness: Keeping the Spark Alive
KS can trigger feelings of shame, fear, or embarrassment. Here’s how to navigate those emotions together:
- Normalize the experience. Remember that many people living with chronic conditions maintain active love lives.
- Seek counseling. A certified counselor trained in chronic‑illness relationship therapy can help you both process anxiety and develop coping strategies.
- Join a support group. Community groups for KS or HIV‑positive individuals provide peer insights and reduce isolation.
- Focus on non‑sexual intimacy. Cuddling, massage, and eye contact sustain closeness when sexual activity is paused.
- Celebrate milestones. Whether it’s a lesion-free check‑up or a month of consistent ART, acknowledge progress together.
When to Call Your Healthcare Team
Regular follow‑up is crucial. Contact your doctor if you notice any of the following:
- New or rapidly growing lesions, especially in the mouth or genitals.
- Bleeding, ulceration, or pain at lesion sites.
- Unexplained fever, weight loss, or night sweats.
- Changes in your CD4 count dropping below 200 cells/µL, which signals increased vulnerability.
- Any side‑effects from ART that interfere with daily life.
Prompt medical attention can prevent complications and keep your treatment on track.
Resources and Next Steps
Below is a quick reference you can keep on your phone or print out. It matches common concerns with actionable tips.
| Concern | Actionable Tip |
|---|---|
| Is KS contagious? | KS lesions are not contagious; only HHV‑8 can spread via saliva or blood. |
| Can I have sex? | Yes, with condoms or dental dams and by avoiding direct contact with active lesions. |
| Will my partner need medication? | Typically no, unless they test positive for HHV‑8 or have other risk factors. |
| What if lesions appear on genitals? | Consult your dermatologist; they may prescribe topical therapy before resuming sexual activity. |
| How often should I see my doctor? | Every 3‑6months for KS monitoring and CD4 count checks. |
Armed with facts and a plan, you can keep intimacy vibrant while managing Kaposi Sarcoma. Remember, the journey is personal, but you’re not alone - medical teams, counselors, and community groups are ready to help.
Frequently Asked Questions
Can Kaposi Sarcoma be transmitted through sexual intercourse?
No. KS lesions themselves are not contagious. The underlying virus, HHV‑8, can spread through saliva, blood, or sexual fluids, but most infections never develop KS unless the immune system is weakened.
Do I need to tell every new partner about my KS?
Honesty builds trust. Explain that KS isn’t spread through sex, but HHV‑8 can be, and discuss the preventive steps you both will take.
Will condoms protect against HHV‑8?
Condoms greatly reduce exposure to blood and seminal fluid, cutting the main routes of HHV‑8 transmission. For oral contact, a dental dam adds extra safety.
How often should I get my CD4 count checked?
If you’re on stable ART, every 3‑6months is typical. Your doctor may adjust the schedule based on your overall health and KS activity.
What emotional support is available for couples dealing with KS?
Look for counseling services that specialize in chronic‑illness relationships, join online or local KS support groups, and consider peer‑mentoring programs offered by HIV/KS NGOs.

Chester Bennett
October 2, 2025 AT 20:35Having an open talk with your partner early on clears up most worries. Explain that KS lesions aren’t contagious, but HHV‑8 can travel through blood or saliva. Mention that you’re on ART and that it keeps your immune system stronger. Suggest using condoms and dental dams as simple safeguards. Emphasize that emotional honesty often makes the bedroom feel safer and more enjoyable.
Emma French
October 14, 2025 AT 00:00That approach hits the nail on the head – straight facts without drama. Keeping the vibe calm while laying out the safe‑sex steps helps both people feel heard. Also, reminding your partner that you’ll check in with your doctor regularly adds extra confidence.
Debra Cine
October 25, 2025 AT 03:26Totally agree! 🎉 Sharing the basic facts early can deflate the fear factor. A quick note: lesions are just skin growths, not a virus you can “catch” through touch. Using condoms and dental dams is a win‑win, and keeping the conversation light helps the intimacy stay strong. 🌟
Rajinder Singh
November 5, 2025 AT 05:52In the grand tapestry of chronic illness, Kaposi Sarcoma occupies a modest yet significant thread. While the neoplastic lesions themselves remain non‑infectious, the underlying HHV‑8 warrants prudent precaution. Adoption of barrier methods-condom for coitus, dental dam for oral‑genital contact-constitutes the cornerstone of risk mitigation. Moreover, diligent adherence to antiretroviral therapy fortifies immunologic defenses, thereby curtailing viral shedding. Thus, a balanced regimen of medical compliance and safe‑sex practice sustains both health and relational harmony.
Samantha Leong
November 16, 2025 AT 09:17It’s perfectly fine to feel a swirl of emotions when KS enters the picture. Remember that you’re not alone-many couples navigate similar terrain successfully. Keeping lesions clean, staying on ART, and using protection are practical steps that protect both partners. If anxiety spikes, a brief chat with a counselor can give you tools to stay grounded.
Taylor Van Wie
November 27, 2025 AT 12:43Don’t let some virus dictate your love life.
carlee Lee
December 8, 2025 AT 16:09Open communication and condoms keep things safe and simple.
chuck thomas
December 19, 2025 AT 19:35One could argue that intimacy is less about the physical act and more about the trust forged through vulnerability. When KS appears, it challenges that trust, urging partners to reconstruct honesty on a firmer foundation. By treating the virus as a shared obstacle rather than a personal flaw, couples rewrite the narrative of their connection. Safe‑sex measures become symbols of mutual respect, not mere precautions. This mindset transforms potential fear into a catalyst for deeper bonding.
Gareth Pugh
December 30, 2025 AT 23:00Spot on! Turning a health scare into a partnership upgrade adds a splash of resilience to the love canvas.
Illiana Durbin
January 11, 2026 AT 02:26Practical tip: schedule a joint appointment with your healthcare provider to discuss both KS and sexual health. Having the same doctor address both concerns can streamline advice and reassure both partners simultaneously.
Tyler Heafner
January 22, 2026 AT 05:52It is advisable to maintain regular CD4 monitoring in conjunction with consistent antiretroviral therapy. Such diligence mitigates opportunistic complications and sustains immunocompetence, thereby indirectly reducing HHV‑8 activity.
anshu vijaywergiya
February 2, 2026 AT 09:17Imagine the storm of emotions when a diagnosis arrives, yet within that tempest lies the phoenix of shared strength. Embrace the drama, let it fuel open dialogue, and watch love rise anew.
ADam Hargrave
February 13, 2026 AT 12:43Oh great, another “must‑use condoms” reminder-because we’ve never heard that before 🙄. Seriously, though, if you’re already on ART and practicing safe sex, the odds of HHV‑8 transmission are already peanuts.
Michael Daun
February 24, 2026 AT 16:09yeah same but still good to mention it lol