Getting the right dose of liquid medicine isn't just about following instructions-it's about staying safe. A wrong measurement can mean the difference between relief and serious harm, especially for children, seniors, or anyone taking multiple medications. The good news? Most liquid prescription labels follow clear, standardized rules designed to prevent mistakes. The bad news? Many people still misread them. If you've ever stared at a bottle and wondered whether 5 mL means one spoonful or five, you're not alone. This guide breaks down exactly what to look for, what it means, and how to measure correctly every time.
Understand the Three Key Parts of the Label
Every liquid prescription label has three essential pieces of information you need to read together:
- Total container volume - This is the total amount of liquid in the bottle, usually printed near the bottom. Common sizes are 118 mL, 237 mL, or 240 mL. This number tells you how much medicine is inside, not how much to take.
- Concentration - This is the most important part. It tells you how much medicine is in each milliliter. Look for something like 125 mg/5 mL. That means every 5 milliliters of liquid contains 125 milligrams of the active drug. If the label says 240 mg/5 mL, then each 5 mL has 240 mg. Never assume the number before the slash is your dose.
- Dosage instructions - This tells you how much to take and how often. It should say something like Take 10 mL twice daily. The number here is always in milliliters (mL), never teaspoons or tablespoons.
Confusing these three parts is the most common cause of dosing errors. For example, if you see a 240 mL bottle and the concentration is 240 mg/5 mL, you might think you’re supposed to take the whole bottle. You’re not. You’re supposed to take 5 mL at a time. Always check the dosage instructions separately from the bottle size and concentration.
Milliliters (mL) Are the Only Safe Unit
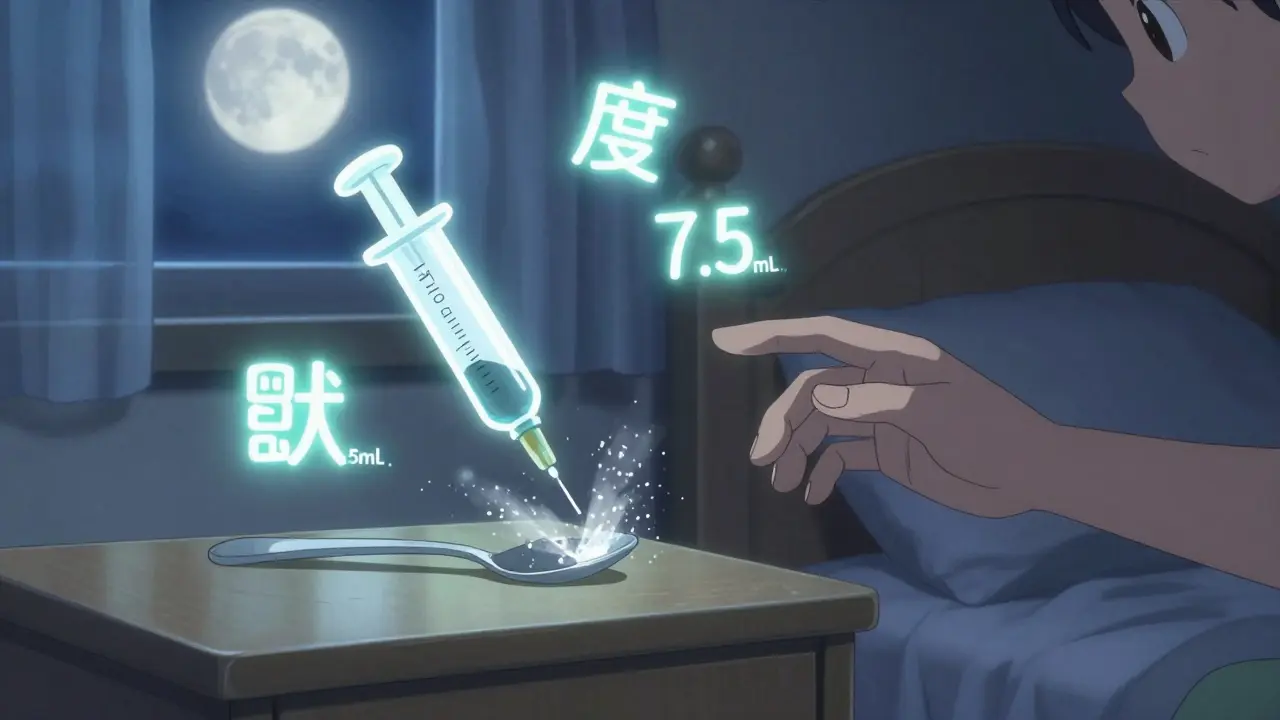
Since 2016, the U.S. Food and Drug Administration (FDA) has required all liquid prescription labels to use milliliters (mL) as the only unit of measurement. This wasn’t just a suggestion-it was a safety rule. Why? Because household spoons are wildly inconsistent.
A teaspoon from your kitchen might hold anywhere from 2.5 mL to 7.5 mL. A tablespoon? It could be 5 mL or 20 mL. A 2018 study by the Consumer Product Safety Commission found that 1 in 4 households used a spoon to give medicine, and over half of those gave the wrong amount. That’s why the National Council for Prescription Drug Programs (NCPDP) banned all references to teaspoons (tsp) or tablespoons (tbsp) on labels. If you see those units printed anywhere on your prescription bottle, it’s outdated-and dangerous.
Modern labels use mL exclusively. The number is always followed by a space before the unit: 5 mL, not 5mL. That small space matters. Studies show it reduces misreading by nearly 20%. And if the dose is less than 1 mL, it must include a leading zero: 0.8 mL, not .8 mL. That tiny zero prevents someone from mistaking 0.8 mL for 8 mL-a 10-fold overdose.
How to Use the Dosing Device
Your prescription should come with a dosing tool: a syringe, cup, or spoon marked in milliliters. Never use a kitchen spoon. Even if it says "teaspoon" on it, it’s not accurate enough.
Here’s what to look for in a good dosing device:
- Clear markings - The mL numbers should be bold, large, and easy to read. The line for your dose should be highlighted or raised.
- Proper range - If your dose is 3.5 mL, your device should measure down to at least 0.1 mL increments. Many pharmacy-provided syringes go as low as 0.01 mL for infants.
- Correct unit - It should only show mL. If it has both mL and tsp, the mL should be larger and more prominent. The tsp markings are there for reference, not for use.
When measuring:
- Place the device on a flat surface.
- Hold it at eye level so the liquid’s surface lines up exactly with your dose line.
- Don’t shake or tilt the device. A slight angle can throw off the measurement by half a milliliter.
- Use the syringe plunger to draw up the exact amount. If using a cup, pour slowly and check twice.
Many pharmacies now include syringes with pediatric prescriptions because they’re more accurate than cups. If yours didn’t come with one, ask for one. Most will give you a free one.
Watch Out for These Common Mistakes
Even with clear labels, people still make the same errors over and over. Here are the top five:
- Confusing concentration with dose - Seeing "240 mg/5 mL" and thinking "I need to take 240 mg, so I’ll give 240 mL." No. The 240 mg is the amount of medicine in 5 mL. If your dose is 120 mg, you need 2.5 mL.
- Misreading decimals - Reading 0.5 mL as 5 mL. Always look for the leading zero. If you see a decimal with no number before it, like ".5 mL," that’s outdated and unsafe.
- Using the wrong device - Using a tablespoon because "it looks right." A tablespoon holds 15 mL. If your dose is 5 mL, you’ve just given three times too much.
- Assuming the bottle size is the dose - A 120 mL bottle doesn’t mean take 120 mL. That’s just how much is in the bottle.
- Not checking the expiration date - Liquid medicines lose potency after opening. Most last 7-14 days once opened, unless the label says otherwise. Never use expired liquid medicine.
A 2021 study from Nationwide Children’s Hospital found that 78% of parents who received a live demonstration from a pharmacist made zero dosing errors. Those who didn’t get help had a 39.4% error rate. That’s not a small gap-it’s life-changing.
Ask for Help-It’s Your Right
You don’t have to figure this out alone. Pharmacists are trained to explain dosing. If you’re unsure, ask them to show you how to measure it. Say: "Can you please show me how to use the syringe? I want to make sure I’m giving the right amount."
Most pharmacies now offer a "teach-back" method: they ask you to demonstrate the dose back to them. This simple step cuts errors by 63%, according to the Agency for Healthcare Research and Quality (AHRQ). If they don’t offer it, ask for it. It’s part of safe medication practice.
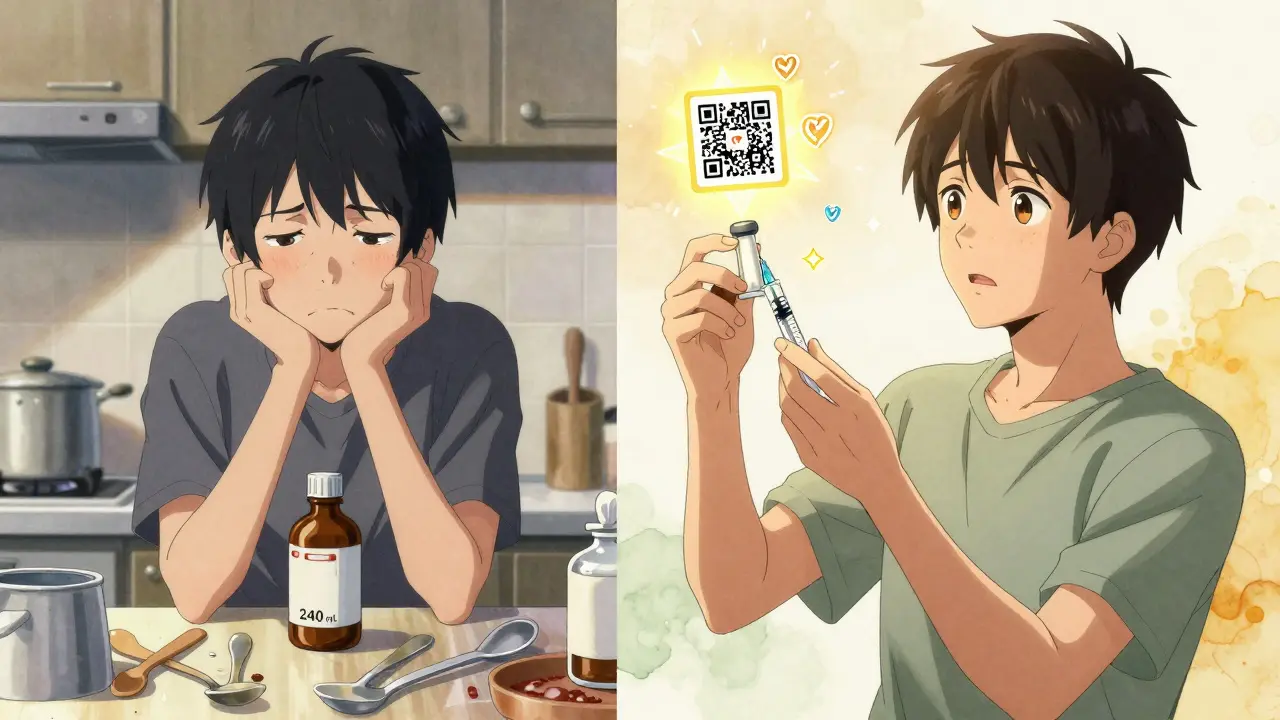
Also, check if your pharmacy gives out printed instructions. If not, ask for them. A written reminder with pictures helps. Many pharmacies now include QR codes on labels that link to short videos showing how to measure the dose. Scan it with your phone. It’s free, easy, and reliable.
What’s Changing in 2026?
By 2026, nearly all pharmacies in the U.S. will be fully compliant with the latest labeling standards. The FDA is pushing for two big updates:
- Pictograms - Simple drawings on labels showing how to use the syringe or cup. A 2022 study in JAMA Internal Medicine showed these reduced errors by 37%.
- QR codes - Scanning the code takes you to a video of a pharmacist demonstrating the exact dose. Amazon Pharmacy and McKesson’s Medly are already using this, and it’s cutting error-related calls by 28%.
These changes aren’t just about technology-they’re about making safety obvious. No more guessing. No more assumptions. Just clear, visual instructions anyone can follow.
Final Checklist Before Giving the Dose
Before you give any liquid medicine, run through this quick checklist:
- Is the dose written in mL, not tsp or tbsp?
- Do I know the concentration (e.g., 160 mg/5 mL)?
- Do I know the exact dose (e.g., 7.5 mL)?
- Am I using the correct device (syringe or cup)?
- Did I check the expiration date?
- Did I measure at eye level?
If you answered yes to all five, you’re safe. If even one is unclear, stop. Call your pharmacy. Wait. Don’t guess.
Why do liquid medicine labels only use mL now?
Liquid medicine labels use only milliliters (mL) because household spoons vary too much in size. A teaspoon can hold anywhere from 2.5 mL to 7.5 mL, making it unreliable for accurate dosing. The FDA and NCPDP mandated mL-only labeling to reduce dosing errors, which are a leading cause of preventable harm in children and seniors. Studies show using mL reduces errors by over 50% compared to using teaspoons or tablespoons.
What if my prescription says "teaspoon" on the label?
If your label still says "teaspoon," it’s outdated. Ask your pharmacist to convert it to milliliters. One teaspoon equals 5 mL, but because kitchen spoons aren’t standardized, you should never rely on them. The pharmacist should give you a proper measuring device and update the label. If they refuse, contact the pharmacy’s manager or file a complaint with your state’s board of pharmacy.
Can I use a regular syringe from the drugstore for medicine?
Yes, but only if it’s labeled for oral use and marked in milliliters. Never use an injectable syringe (the kind with a needle) for medicine. Oral syringes have a wide tip and no needle, and they’re designed for safe, accurate dosing. Most pharmacies give them out for free with liquid prescriptions. If you need one, ask for it-no prescription required.
How do I know if I’m giving too much or too little?
Always double-check the concentration and the dose. For example, if the label says 125 mg/5 mL and your dose is 10 mL, you’re giving 250 mg total. If you accidentally gave 15 mL, that’s 375 mg-50% more than prescribed. Signs of overdose include drowsiness, vomiting, or unusual behavior. Signs of underdose include no improvement in symptoms. If you’re unsure, call your doctor or pharmacist immediately. Never wait to see if "it’ll fix itself."
What should I do if my child spits out part of the dose?
Don’t give another full dose. Call your pharmacist or doctor. If your child spit out most of it (more than half), they may need another full dose. If it was only a small amount, they likely got enough. Giving extra medicine can lead to overdose. Always ask for guidance-don’t guess.
Next Steps for Safer Medication Use
Keep your liquid medicines in a central location, away from children and heat. Always check the expiration date before each use. Store syringes and cups separately from other tools-don’t mix them with kitchen utensils. If you’re managing multiple medications, write down each dose and time on a calendar. Many pharmacies offer free medication organizers with printed labels.
For parents: Ask your pediatrician to review dosing during every well-child visit. For seniors: Have a family member or caregiver help you double-check doses. For anyone: If you’re ever confused, call your pharmacy. They’re paid to help you get this right.
Medication safety isn’t about being perfect. It’s about being careful. And the best way to be careful is to know exactly what the label says-and never assume anything.

Jack Havard
February 12, 2026 AT 10:48The FDA mandates mL only? Funny how they suddenly care about safety after decades of letting people die from spoon dosing. They didn't ban sugar in kids' meds, didn't stop pharmaceutical companies from making flavors that taste like chemical candy, and yet now they're obsessed with a space before 'mL'? This is performative regulation. Real safety would be standardized dosing devices in every pharmacy, not a punctuation rule that does nothing for the 80% of people who still use kitchen spoons anyway.
Annie Joyce
February 12, 2026 AT 20:23I love how this guide breaks it down like a real human would. I used to give my son his antibiotic with a teaspoon until I read this-now I keep a syringe in my wallet. Seriously. I’ve got one in my purse, one in the car, and one taped to the fridge. The leading zero thing? Game changer. I once thought .5 mL was 5 mL. Nearly panicked when I realized. Don’t let your meds be a guessing game. Get the syringe. Ask for help. It’s not embarrassing-it’s smart.
Steve DESTIVELLE
February 12, 2026 AT 21:01The obsession with milliliters reveals a deeper epistemological failure in modern medicine. We have reduced the sacred act of healing to a quantifiable metric because we fear the ineffable. The body does not respond to mL-it responds to intention. To trust a syringe over instinct is to surrender autonomy to a system that profits from confusion. The real problem is not the label-it is the alienation of care from the home. A mother’s touch, a grandmother’s intuition, these are the true dosimeters. We have replaced wisdom with calibration. And in doing so we have made the sick more afraid than cured.
Stephon Devereux
February 14, 2026 AT 12:10This is exactly the kind of practical wisdom we need more of. Seriously-how many people have overdosed their kids because they thought a 'teaspoon' meant the one from their kitchen? I used to be one of them. I didn’t know the difference between concentration and dose until my niece got sick after I gave her the wrong amount. Don’t assume. Don’t guess. Ask. Use the syringe. Check the expiration. Measure at eye level. These aren’t just tips-they’re survival tactics. And if your pharmacy doesn’t give you a free syringe? Go somewhere else. Your life isn’t worth cutting corners.
steve sunio
February 16, 2026 AT 05:39Neha Motiwala
February 18, 2026 AT 01:10Wait wait wait-I just realized something terrifying. What if the QR code gets hacked? What if the video is replaced with a fake pharmacist telling you to give 10x the dose? What if the FDA is using this to track your medication use? And don’t even get me started on the syringes-how do we know they’re not laced with microchips? I’ve been using my coffee spoon for years and my kid’s fine. Maybe the system wants us dependent on devices so they can control us. I’m calling my pharmacist right now. I need to know who printed this label. I need proof. I need to see the original paperwork. I’m not giving my child anything until I have a notarized affidavit.
athmaja biju
February 18, 2026 AT 16:51In India, we have been measuring medicine with teaspoons for generations. Our ancestors did not need QR codes or syringes. Our medicine was made from herbs, not corporate chemicals. This Western obsession with milliliters is a form of cultural imperialism. We know our bodies. We know our children. You think a plastic syringe from America is safer than a grandmother’s intuition? You think a label written by a corporate lawyer is more trustworthy than a family’s lived experience? This is not progress. This is control disguised as safety. We do not need your syringes. We need our traditions back.
Robert Petersen
February 20, 2026 AT 08:29Just wanted to say thank you for writing this. Seriously. I’ve been a nurse for 18 years and I still see parents panic over these labels. This guide is clear, calm, and kind. No jargon. No condescension. Just facts with heart. I’m printing this out and taping it to the wall at my clinic. If you’re reading this and you’re unsure-don’t be ashamed. Ask. Call. Text. Send a photo. Someone will help you. You’re not alone. And you’re not stupid. You just didn’t know. Now you do. That’s all that matters.