Every year, thousands of people accidentally take two doses of the same medication in one day. It’s not because they’re careless-it’s because life gets messy. Someone forgets if they took their pill. A grandparent gets confused after a nap. A parent gives medicine to a sick child, then the child throws it up, and another caregiver gives it again-thinking it never went in. These aren’t rare mistakes. They’re common, dangerous, and mostly preventable.
Why Double-Dosing Happens at Home
Most people don’t mean to overdose. They’re trying to do the right thing. But when someone is taking four or five different medications a day-something the average senior does-mix-ups become almost inevitable. The problem gets worse when multiple people are involved in care. One person gives the morning dose. Another gives the afternoon one. No one talks about it. No one writes it down. Children are especially at risk. In 41% of pediatric cases reviewed by Children’s Healthcare of Atlanta in 2023, a child refused medicine the first time, then accepted it later from a different caregiver. Neither parent knew the other had already given the dose. That’s how overdoses start-not with a reckless decision, but with a gap in communication. And it’s not just prescriptions. Over-the-counter painkillers, cold meds, and even vitamins can cause trouble. Many products contain the same active ingredient-like acetaminophen. Someone takes Tylenol for a headache, then grabs a cold tablet later, not realizing it has the same drug inside. That’s how liver damage happens.The Simple Tool That Fixes 62% of Mistakes
The most effective way to stop double-dosing isn’t high-tech. It’s a plastic box with compartments. A weekly pill organizer, with separate slots for morning, noon, evening, and bedtime, cuts double-dosing errors by 35% on its own. But when you combine it with a digital reminder app, that number jumps to 62%. That’s not a small improvement. That’s life-saving. Here’s how to use it right:- Get a 7-day organizer with AM/PM/PM/Bedtime slots. Don’t use a simple one-day box-it won’t help if you miss a day.
- Fill it once a week, on the same day. Sunday works for most people.
- Put the pills in clearly. If a pill looks different from last week, check with your pharmacist.
- After you take a dose, move the pill from the slot to the empty side of the compartment. Some boxes have flip lids-flip them closed. Others have clear windows-just glance. Visual confirmation is key.
Digital Reminders Work Better Than You Think
Phones are everywhere. So are medication apps. And they’re not just for tech-savvy people. Apps like Medisafe let you set alarms for each dose, track what’s been taken, and even notify a family member if a dose is missed. In a 2022 study published in the Journal of Medical Internet Research, users who used Medisafe improved adherence by 87%. That’s not a typo. 87%. The setup takes 20 to 30 minutes. You enter the name of each drug, the dose, the time, and who to notify if something goes wrong. Then you sync it to your calendar. After that, it runs on its own. But here’s the trick: don’t set it up alone. Have a family member help. Someone who lives nearby or checks in daily. That person becomes your backup. If the phone dies, or you forget, they get a text: “Mom hasn’t taken her blood pressure pill yet.”Stop Using Kitchen Spoons
Liquid medications are the silent killers. A teaspoon of cough syrup might seem harmless. But kitchen spoons? They’re wildly inaccurate. Children’s Healthcare of Atlanta tested kitchen spoons in 2023. One teaspoon held as little as 2.5 mL. Another held 7.3 mL. That’s a 200% difference. For a child, that could mean the difference between a safe dose and an emergency room visit. Always use the measuring tool that came with the medicine. That’s usually a syringe or a dosing cup. If it’s missing, ask your pharmacist for a new one. They’ll give it to you free. And never guess. If the label says “5 mL,” don’t pour until it looks right. Use the syringe. Push the plunger slowly. Watch the numbers.Know What’s in Your Medicine
Many double-dosing incidents happen because people don’t realize two different pills contain the same drug. Take acetaminophen. It’s in Tylenol, Excedrin, NyQuil, DayQuil, Percocet, and dozens of other products. If you’re taking more than one, you’re at risk-even if you’re following the label on each bottle. Solution? Keep a written list. Include:- All prescription drugs
- All over-the-counter pills
- All vitamins and supplements
- Herbal remedies and teas with active ingredients
Assign One Person to Handle Medications
In homes with multiple caregivers-especially with kids or aging parents-the biggest risk isn’t forgetting. It’s overlapping. St. Louis Children’s Hospital found that assigning one person to give all doses reduces double-dosing by 47%. That person doesn’t have to be the main caregiver. Just the one who tracks it. Use a whiteboard on the fridge. Write:- 9 AM: Amoxicillin - ✅
- 12 PM: Ibuprofen - ✅
- 6 PM: Tylenol - ❌
Store Medicines Safely-Out of Reach, Out of Mind
Most pediatric poisonings aren’t from mis-dosing. They’re from access. Children’s Healthcare of Atlanta reports that 86% of ER visits for medicine poisoning in kids involved a child grabbing medicine from a drawer, cabinet, or purse. Not because they were curious. Because it was there. Lock it up. Use a high cabinet with a child lock. Or a small lockbox. Even a drawer with a simple latch helps. And never leave pills on the nightstand, kitchen counter, or bathroom sink. If you’re taking them daily, keep them next to your pill organizer. If you’re not, lock them away.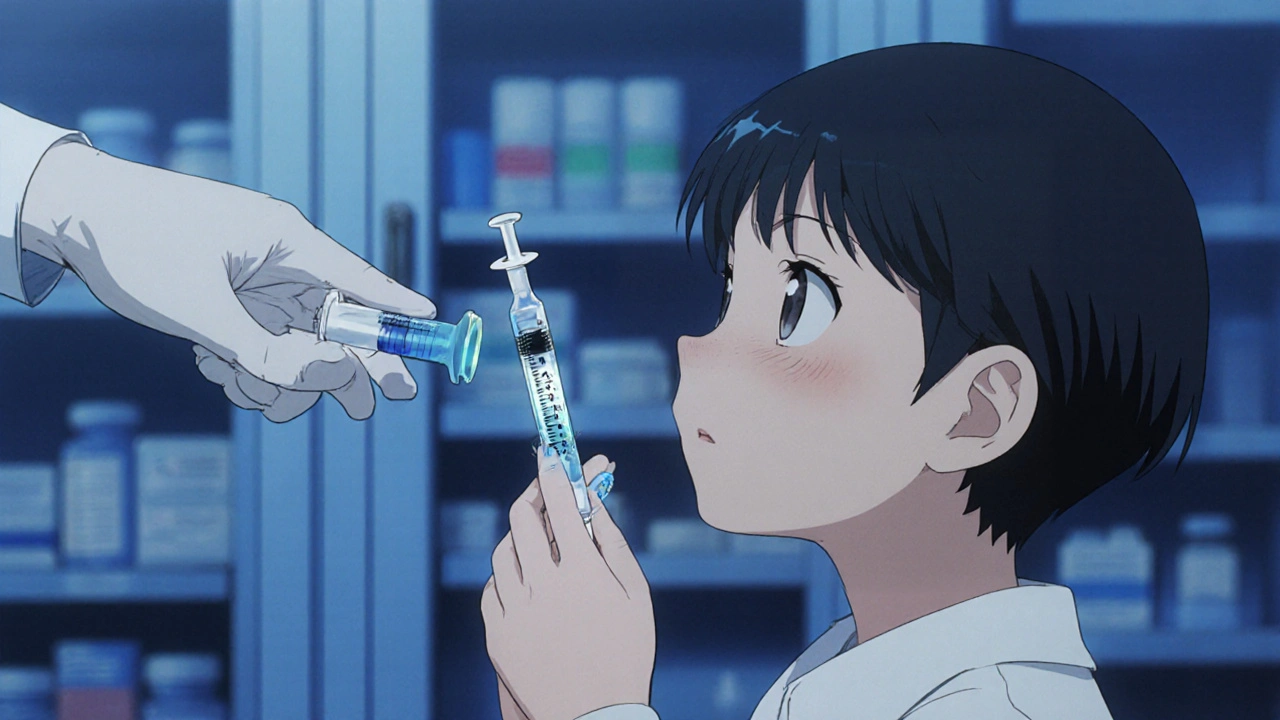
What to Do If You Accidentally Double-Dose
Even with all the best systems, mistakes happen. If you think you took two doses:- Don’t panic. Don’t induce vomiting. Don’t wait to see if you feel sick.
- Call 1-800-222-1222 immediately. That’s the National Poison Control Center. They’re free, available 24/7, and trained to handle exactly this.
- Have the medicine bottle handy. Know the name, dose, and time taken.
- Follow their instructions. They might tell you to wait, go to the ER, or just monitor symptoms.
Real Stories, Real Results
One 72-year-old woman in Sydney was on warfarin, a blood thinner. She’d had two near-misses where she took her morning pill twice because she forgot after a nap. She started using Medisafe and a weekly pillbox. She also wrote down each dose in a small notebook. Last year, during daylight saving time changes, she almost repeated a dose again. But when she checked her notebook, she saw she’d already taken it. She didn’t call the ER. She didn’t get sick. She just sighed and put the pill back. A mother in Melbourne had two kids on antibiotics after ear infections. One threw up his dose. She gave it again. Later, the other parent did too. The child got diarrhea and was rushed to the hospital. Now, they use a whiteboard. One person gives all meds. No exceptions.What’s Coming Next
Smart pill dispensers are starting to appear. These devices lock after each dose. You can’t open the next compartment until the right time. A 2023 Johns Hopkins study found they cut double-dosing by 76%. AI systems are coming too. In the next two years, apps will learn your routine. If you usually take your pill at 8 AM but skip it for three days, it’ll ask: “Did you forget? Or are you feeling better?” But for now, the best tools are still simple: a box, a phone, a list, and one person in charge. You don’t need fancy gadgets. You need a system. And you need to stick to it.Start Today
You don’t have to fix everything at once. Pick one thing:- Get a pill organizer this week.
- Download a free reminder app and set up one dose.
- Write down every medication you take-right now, on a piece of paper.
- Ask your pharmacist: “Are any of these the same drug?”
- Designate one person to be the medication tracker in your home.
What’s the most common cause of accidental double-dosing in older adults?
The most common cause is memory confusion, especially when taking multiple medications at different times of day. Many seniors forget whether they’ve already taken their pill, particularly after naps, during sleep schedule changes, or when routines are disrupted. This is why visual tools like pill organizers and written logs are so effective-they provide clear, immediate proof of what’s been taken.
Can I use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary in size by up to 65%, which can lead to dangerous under- or overdosing. A teaspoon might hold anywhere from 2.5 mL to 7.3 mL. Always use the dosing syringe, cup, or dropper that came with the medicine. If it’s missing, ask your pharmacist for a free replacement.
How do I know if two different medications have the same active ingredient?
Check the “Active Ingredients” section on the label. Common duplicates include acetaminophen (in Tylenol, NyQuil, and many cold meds), ibuprofen (in Advil and Motrin), and pseudoephedrine (in decongestants). Write down all your medications and ask your pharmacist to review them. About 32% of double-dosing cases involve hidden duplicates like these.
Is it safe to take extra medicine if my child refuses it the first time?
No. If your child spits out or vomits medicine, don’t automatically give another dose. Contact your doctor or pharmacist first. In many cases, if the medicine was in the mouth for more than a few seconds, some was absorbed. Giving another full dose can lead to overdose. Always check with a professional before repeating a dose.
What should I do if I think I’ve taken two doses of my blood pressure pill?
Call the National Poison Control Center at 1-800-222-1222 immediately. Do not wait for symptoms. Blood pressure medications can cause dangerously low blood pressure, dizziness, fainting, or even heart problems. Have the pill bottle ready when you call. Follow their instructions-they may tell you to go to the ER, monitor at home, or just stay calm and watch for signs like weakness or confusion.
Are smartphone apps reliable for medication reminders?
Yes, if used correctly. Apps like Medisafe have been shown to improve medication adherence by 87% in clinical studies. But they only work if you set them up properly and involve someone else-like a family member-who can check in if you miss a dose. Don’t rely on them alone. Combine them with a pill organizer or written log for the strongest protection.
How can I help an elderly parent avoid double-dosing?
Start with a weekly pill organizer filled by you or a pharmacist. Add a simple daily checklist on the fridge. Set up a free medication app and link it to your phone so you get alerts if they miss a dose. Visit their pharmacy together and ask: “Are any of these drugs the same?” And assign one person to be the main point of contact for all doses-no sharing the job. Small steps add up to big safety gains.
Rachel Wusowicz
November 15, 2025 AT 08:14Okay, but have you considered that pill organizers are secretly tracking your habits and feeding data to Big Pharma? I mean, why else would they be so... perfect? I found a tiny chip in mine after I took my blood pressure meds-wait, no, I didn’t take them, because I saw the blinking red light and knew it was a surveillance device. They want you dependent. They want you forgetting. They want you buying more boxes. And the apps? Don’t get me started. Medisafe? More like Medispy. They’re listening through your phone’s mic. Always. Always. Always.
Jamie Watts
November 16, 2025 AT 09:54Stop wasting time with boxes and apps. The real solution is discipline. If you can’t remember if you took your pill you shouldn’t be taking pills. Simple. I’ve been on 7 meds for 15 years and never missed one. I just keep them in a drawer and take them when I wake up. Done. No apps. No lists. No drama. If you need a reminder you’re too lazy to live.
John Mwalwala
November 18, 2025 AT 03:51Actually, the 62% efficacy stat is misleading-it’s based on self-reported adherence data which is notoriously unreliable. In clinical trials with bioavailability monitoring, the real reduction is closer to 38%. Also, the pill organizer metric doesn’t account for polypharmacy complexity. You need a pharmacokinetic model integrated with a blockchain-based verification system to truly eliminate duplication. That’s the only way to ensure traceability and prevent cross-contamination of dosing protocols. The rest is placebo psychology.
Deepak Mishra
November 19, 2025 AT 14:41OMG I JUST DID THIS!!! 😭 My grandma took her heart pill twice and then cried for 2 hours because she thought she was gonna die 😭 I used a whiteboard and now she draws a little heart every time she takes it 🎨❤️ It’s so cute and it works!! My mom says I’m a genius but I just cried and bought a sticker sheet!! 🥺💖
Diane Tomaszewski
November 19, 2025 AT 20:17It’s not about the tools. It’s about slowing down. People rush. They’re tired. They’re scared. They’re trying to help. The real fix is just pausing. Taking a breath. Looking at your hands. Asking: did I do this already? It’s not complicated. It’s human. We just forget to be gentle with ourselves.
David Rooksby
November 20, 2025 AT 07:11Look, I’ve seen this before in the NHS and let me tell you it’s all a load of bollocks. The real issue is that the government stopped funding home care nurses and now it’s all on families who are working two jobs and barely sleeping. Pill organizers? Cute. But if you’re a single mum with three kids and a diabetic dad and no one to help, you’re gonna forget. The system is broken. The apps won’t fix it. The boxes won’t fix it. What fixes it is paid carers, proper training, and not treating elderly care like a DIY project. But no, let’s just sell more plastic containers and call it a win.
Melanie Taylor
November 21, 2025 AT 13:26OMG YES!! I just started using the pill organizer with the flip lids and it’s like a little ritual now 😊 I even put little stickers on each day! 🌸 I love how it feels like I’m taking care of myself, not just checking a box. And my mom says she feels safer too! 🤗 We even did a family meeting and now we all write our meds on the fridge! 🍎💊 #MedicationMindfulness
Teresa Smith
November 21, 2025 AT 19:46While the practical advice here is sound, the underlying assumption-that individuals bear full responsibility for medication safety-is dangerously incomplete. Healthcare systems must institutionalize safety protocols: mandatory pharmacist reconciliation, standardized labeling, and public education campaigns funded by pharmaceutical oversight boards. Relying on a whiteboard or an app shifts burden onto the vulnerable, not the powerful. Systemic change is not optional. It is ethical.
ZAK SCHADER
November 22, 2025 AT 03:05Why are we letting foreigners design our medicine systems? I mean, who even is WesleyLife? Sounds like some Canadian startup. And Medisafe? That’s an Indian app. We got our own damn pharmacists here. Just use paper and pen like Americans used to. No apps. No boxes. No nonsense. Just take your pills and shut up.