Obesity & Vascular Risk Calculator
Assess Your Vascular Risk
Enter your basic measurements to see how obesity affects your vascular health
Quick Takeaways
- Obesity raises the chance of vascular disease by 2‑3× through inflammation, insulin resistance and lipid changes.
- Key pathways include endothelial dysfunction, high blood pressure and atherosclerotic plaque buildup.
- Weight loss of 5‑10% can reverse many early vascular changes.
- Combining diet, regular activity and medical treatment lowers risk better than any single approach.
- Seek professional advice if you have a BMI≥30kg/m², persistent hypertension, or unexplained leg pain.
What the link really means
When people talk about the link between Obesity is an excess accumulation of body fat that raises the risk of chronic diseases and vascular disease is any disorder that impairs the arteries, veins or capillaries, often leading to heart attacks, strokes or peripheral artery disease, they’re not just tossing around buzzwords. The extra fat tissue acts like a chemical factory, releasing substances that poison blood‑vessel walls and mess with metabolism.
In plain terms, the heavier you get, the more strain you put on your circulatory system, and the higher the odds that a blockage or rupture will occur.
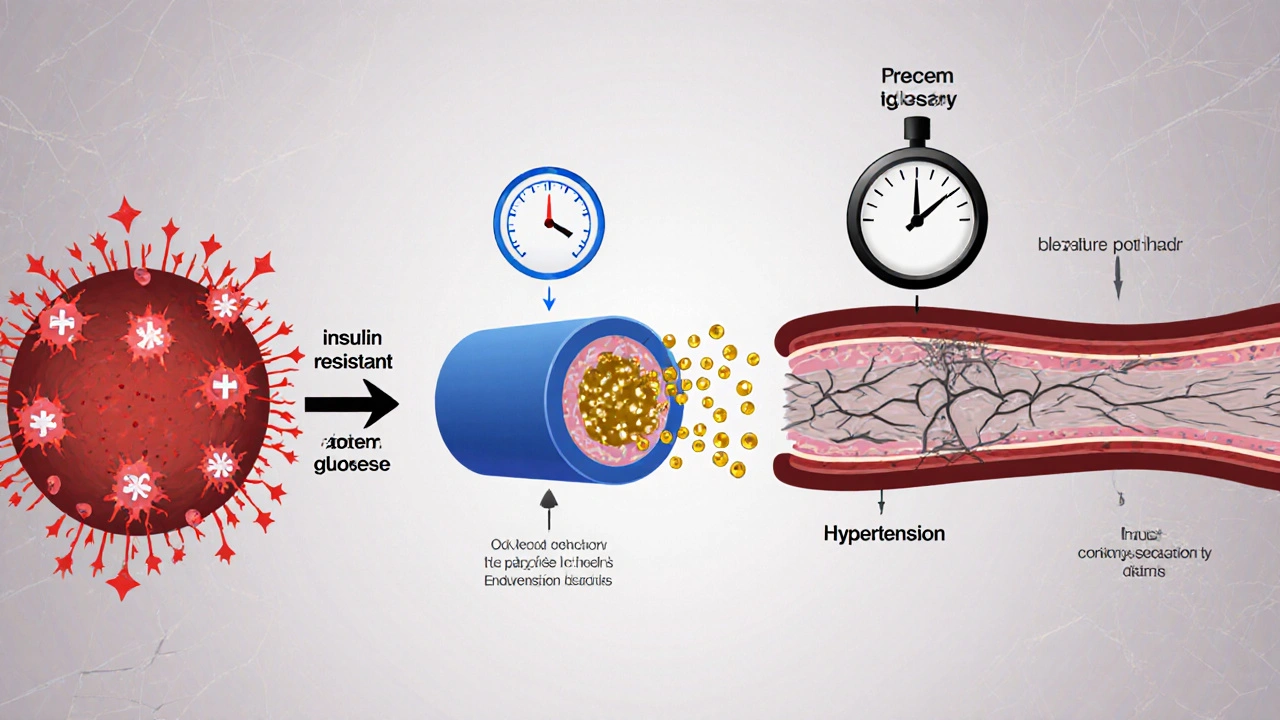
Biological pathways that connect the two
Four major mechanisms drive the obesity‑vascular disease connection:
- Chronic low‑grade inflammation - Fat cells, especially around the abdomen, secrete inflammation is a sustained immune response marked by cytokines like IL‑6 and TNF‑α that damages blood‑vessel lining. This irritates the endothelium and accelerates plaque formation.
- Insulin resistance and type2 diabetes - Excess weight makes body cells less responsive to insulin, leading to higher blood sugar. Elevated glucose triggers oxidative stress and promotes cholesterol is a fatty molecule that, when oxidized, sticks to artery walls forming plaques abnormalities.
- Elevated blood pressure - More mass means the heart pumps harder, raising arterial pressure. Hypertension strains the endothelium, making it easier for plaques to rupture.
- Endothelial dysfunction - The inner lining of blood vessels loses its ability to relax and regulate clotting, a direct result of the chemical cocktail released by excess fat.
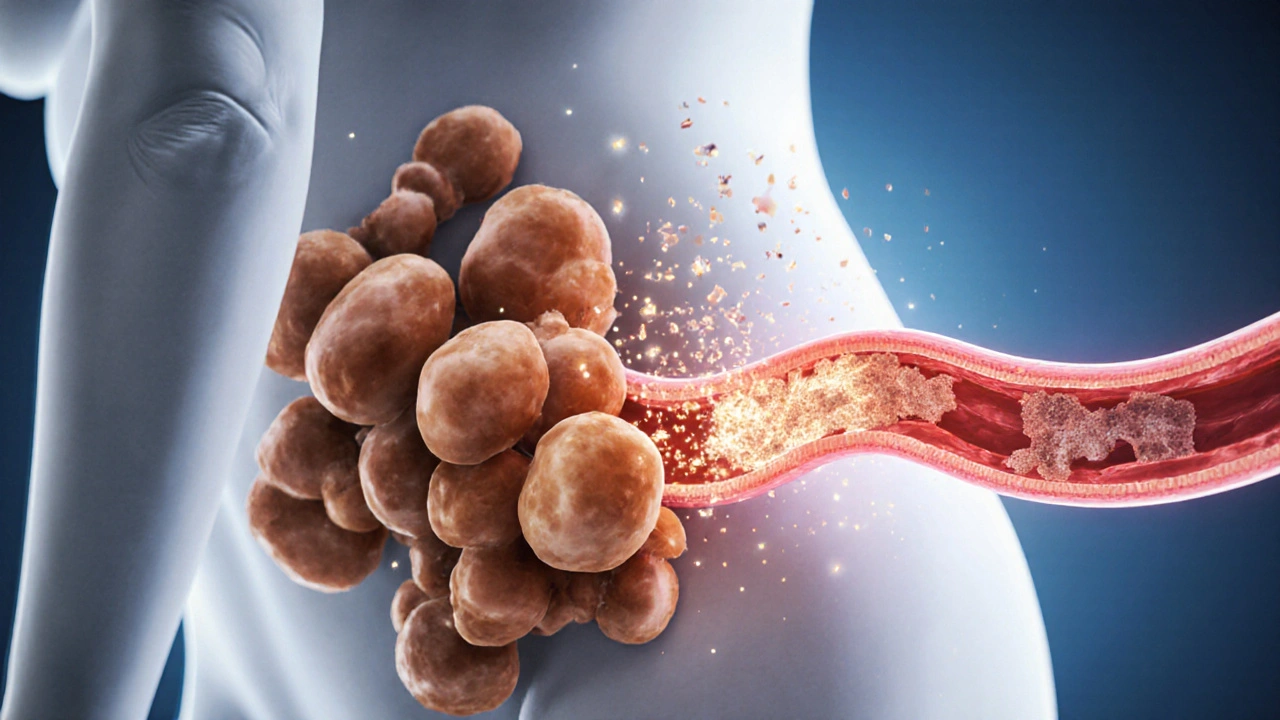
Vascular conditions most affected by obesity
Obesity doesn’t just boost the odds of one disease; it amplifies several serious vascular problems:
- atherosclerosis is the buildup of fatty plaques inside arteries that narrows the lumen and can cause heart attacks or strokes
- hypertension is persistently high arterial pressure that strains the heart and damages small vessels
- Peripheral artery disease (PAD) - Reduced blood flow to the legs, leading to pain while walking.
- Aneurysms - Weakening of arterial walls that may rupture under pressure.
Studies from the UK Biobank (2023) show that participants with a BMI≥35kg/m² had a 2.5‑fold higher risk of developing atherosclerotic coronary disease than those with a BMI<25kg/m².
How to spot early warning signs
Vascular disease often hides until a major event occurs. Look out for:
- Chest discomfort or shortness of breath during mild activity.
- Sudden vision changes or headaches - possible signs of carotid artery narrowing.
- Leg cramping or numbness when walking short distances (PAD).
- Persistent high blood pressure readings (≥140/90mmHg).
If any of these appear alongside a BMI≥30kg/m², it’s time to schedule a cardiovascular check‑up.
Practical lifestyle moves that work
Weight loss isn’t a magic bullet, but shedding even a modest amount can reverse early vascular damage.
obesity‑related inflammation drops by roughly 30% after a 5% reduction in body weight.
- Diet revamp - Aim for a Mediterranean‑style plate: ½ vegetables, ¼ lean protein (fish, legumes), ¼ whole grains, plus olive oil. This pattern cuts LDL‑cholesterol by 10‑15% and improves endothelial function.
- Move daily - 150 minutes of moderate aerobic activity (brisk walking, cycling) per week plus two strength‑training sessions lowers systolic blood pressure by 5‑8mmHg.
- Quit smoking - Tobacco multiplies the vascular risk of obesity by up to three times.
- Sleep hygiene - 7‑8 hours of quality sleep helps regulate hormones that control hunger (ghrelin) and fullness (leptin).

Medical options when lifestyle isn’t enough
Doctors may prescribe or recommend the following:
- Statins - Lower LDL‑cholesterol, stabilise plaques, and modestly reduce inflammation.
- ACE inhibitors or ARBs - Control blood pressure and improve endothelial health.
- bariatric surgery is a set of gastrointestinal procedures that reduce stomach size, leading to rapid, sustained weight loss - Patients lose an average of 25‑30% of excess weight, with a 60‑70% reduction in cardiovascular events over five years.
- GLP‑1 receptor agonists - New diabetes drugs that also promote weight loss and improve blood‑vessel function.
Choosing a treatment depends on BMI, existing comorbidities, and personal preferences. A shared decision‑making conversation with a cardiologist or endocrinologist is essential.
Comparing obesity’s impact on three major vascular diseases
| Condition | Relative Risk (BMI≥30) | Typical Age of First Event | Key Preventive Measure |
|---|---|---|---|
| Atherosclerotic coronary disease | 2.5× | 45‑60years | Statin + 5‑10% weight loss |
| Hypertension | 1.8× | 30‑50years | Salt reduction + regular exercise |
| Peripheral artery disease | 2.0× | 55‑70years | Walking program + smoking cessation |
Monitoring and when to see a professional
Regular check‑ups keep the problem in view:
- Annual lipid panel and fasting glucose.
- Blood pressure at each primary‑care visit.
- Body‑mass index (BMI) calculation; aim for < 25kg/m² if possible.
- Ask for a peripheral‑pulse exam if you notice leg pain.
If you experience any chest pain, sudden vision loss, or severe shortness of breath, treat it as an emergency and call 999.
Frequently Asked Questions
Can a normal‑weight person still develop vascular disease?
Yes. Genetics, smoking, high‑salt diet and sedentary lifestyle can cause vascular problems even without excess weight, but obesity adds a substantial extra risk.
How quickly can vascular health improve after losing weight?
Studies show measurable improvements in endothelial function within 3‑6 months of a 5‑10% body‑weight reduction, and blood pressure often drops within a few weeks.
Is bariatric surgery worth the risk for heart health?
For people with BMI≥35 and at least one cardiovascular risk factor, surgery reduces major heart events by up to 70% over five years, outweighing the operative risks in most cases.
What role does diet quality play compared to calorie count?
Quality matters because foods high in saturated fat and refined carbs worsen lipid profiles and inflammation, even if total calories are modest. A Mediterranean diet improves both weight loss and vascular markers.
Are there non‑invasive tests to detect early vascular damage?
Carotid‑intima media thickness (CIMT) ultrasound, ankle‑brachial index (ABI) for PAD, and flow‑mediated dilation (FMD) are reliable, low‑risk methods to spot early arterial changes.
Kim and Lin
October 12, 2025 AT 14:25Obesity is a ticking time bomb for your arteries, get your act together! >:)
Veronica Mayfair
October 19, 2025 AT 13:05Hey folks! 🌟 This article breaks down why extra pounds can mess with your blood vessels, and honestly it’s a good wake‑up call. I love how it shows the simple math: lose 5‑10% of weight and you could reverse early damage. Remember, staying active doesn’t have to mean marathon training – a daily walk does wonders. Let’s keep supporting each other on this journey, you got this! 🙌
Rahul Kr
October 26, 2025 AT 10:45Interesting read. The inflammation bit really hits home – my uncle’s hypertension got worse after he stopped exercising. It’s a reminder that even a small lifestyle tweak can help. Definitely worth keeping an eye on those waist numbers.
Anthony Coppedge
November 2, 2025 AT 09:25There is a clear, mechanistic link between excess adiposity and vascular pathology, and the article does an admirable job of outlining each pathway. First, chronic low‑grade inflammation, mediated by cytokines such as IL‑6 and TNF‑α, damages endothelial integrity; this is a well‑documented precursor to atherogenesis. Second, insulin resistance escalates circulating glucose, fostering oxidative stress that further destabilizes plaques. Third, the hemodynamic load imposed by higher body mass forces the heart to work harder, thereby elevating systolic and diastolic pressures. Fourth, endothelial dysfunction diminishes nitric oxide bioavailability, impairing vasodilation and promoting a pro‑thrombotic state. Moreover, the synergistic effect of these mechanisms compounds risk, making obesity a potent multiplier for cardiovascular events. The calculator presented here is useful for personal risk assessment, though it should be complemented by professional medical evaluation. Lifestyle interventions – particularly a 5‑10% weight reduction – can dramatically improve these parameters, as multiple randomized trials have shown. Dietary modifications, regular aerobic activity, and, when necessary, pharmacologic therapy together offer the most comprehensive risk mitigation strategy. It is also worth noting that waist‑to‑hip ratio adds predictive value beyond BMI alone, especially in distinguishing visceral fat distribution. In practice, clinicians should incorporate both metrics when counseling patients. Finally, public health initiatives that promote healthier eating environments and active transportation are essential to curb the rising tide of obesity‑related vascular disease. Overall, this piece reinforces the urgent need for both individual and systemic action to address the intertwined epidemics of obesity and cardiovascular disease.
Tim Ferguson
November 9, 2025 AT 08:05Honestly, I think all these calculators are just gimmicks – you can’t capture the whole picture with a few numbers.
Brian Jones
November 16, 2025 AT 06:45Wow, a 15‑sentence dissertation on a simple risk tool – talk about over‑engineering!; but hey, if it helps people realize they need to move a bit more, why not?
Narayan Iyer
November 23, 2025 AT 05:25Yo fam, this stuff is legit – the metabolic syndrome cascade is like a chain reaction in the body, ya know? When you stack on the adipose, you’re basically feeding the inflammatory cytokine factory, which then messes up insulin signaling and spikes that blood pressure. So, dropping even a couple of kilos can break that loop and give your endothelium a breather. Keep it real, stay active, and don’t let the lab data scare you – use it as a roadmap.
Gary Smith
November 30, 2025 AT 04:05We Americans need to stop sugar‑coating this – obesity is a national emergency, and it’s ruining our arteries!!
Dominic Dale
December 7, 2025 AT 02:45The government isn’t telling you the full story; they’re hiding how big pharma benefits from keeping the population overweight. Think about it – the more people with hypertension, the more prescriptions get written, the more profit streams are open. And the media just spins these health calculators as if they’re neutral tools, ignoring the hidden agenda. Even the research funding is steered by lobbying groups that want to maintain the status quo. It’s a perfect storm of corporate interests, policy complacency, and public complacency. If we wanted to fix this, we’d have to dismantle that entire ecosystem, which is why you rarely see genuine solutions offered. Stay vigilant and question the narratives fed to you.
christopher werner
December 14, 2025 AT 01:25I respect the passion, but let’s keep the discussion factual and avoid unfounded accusations.
Matthew Holmes
December 21, 2025 AT 00:05Whoa... this really blows my mind, like the whole thing is a massive conspiracy to keep us sick but we’re finally seeing the truth!