What Exactly Is Gout?
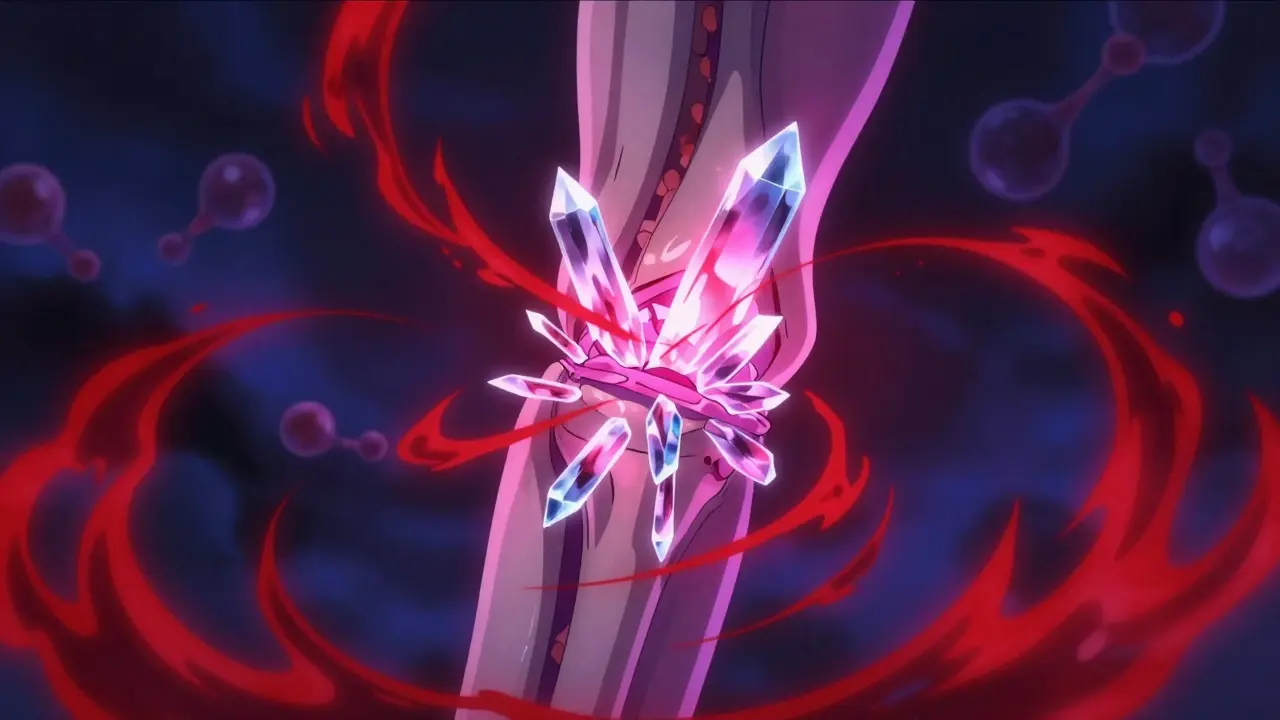
Gout isn’t just a bad joint ache. It’s a disease caused by crystals forming inside your joints-crystals made from uric acid. These sharp, needle-like crystals trigger intense inflammation, swelling, and pain, often hitting the big toe first. But it can also show up in ankles, knees, fingers, and elbows. About 8.3 million Americans have it, and it’s not going away. In fact, cases have jumped 47% since 1990. The root cause? Too much uric acid in the blood. That’s called hyperuricemia, and it happens when your body either makes too much uric acid or can’t flush it out properly.
Where Does Uric Acid Come From? (The Purine Connection)
Your body breaks down purines-natural substances found in your cells and in certain foods-to make energy. When purines are used up, they turn into uric acid. Humans are unique: we lost the enzyme uricase about 15 to 20 million years ago. That enzyme used to turn uric acid into something harmless that your body could easily remove. Without it, uric acid builds up. About 65% of it leaves through your kidneys, and 35% goes through your gut. But here’s the problem: your kidneys reabsorb 90% of the uric acid they filter. That means even if you’re trying to flush it out, most of it gets pulled right back in. This is why simply drinking more water won’t fix gout on its own.
Purines come from two places: your body’s own cells (about 80%) and what you eat (about 20%). That’s why people think gout is just from eating too much steak or seafood. But even if you eat perfectly, your body can still overproduce uric acid because of how your enzymes work. For example, if you have a rare genetic condition called Lesch-Nyhan syndrome, you’re missing an enzyme called HPRT, and your body makes way too much uric acid. Even without that, small changes in how your enzymes handle purines can push you into gout territory.
When Does Uric Acid Become Dangerous?
The magic number is 6.8 mg/dL. That’s the point where uric acid starts to crystallize in your joints. If your blood level stays above 7.0 mg/dL, your risk of gout jumps dramatically. At 9.0 mg/dL or higher, nearly 28% of people will develop gout. That’s not a small risk-it’s a guarantee if nothing changes. The American College of Rheumatology says if you’ve had even one gout attack, you need to lower your uric acid to below 6.0 mg/dL. If you have visible tophi (those lumps of crystals under your skin), you need to get it even lower-below 5.0 mg/dL. That’s not a suggestion. That’s medical necessity.
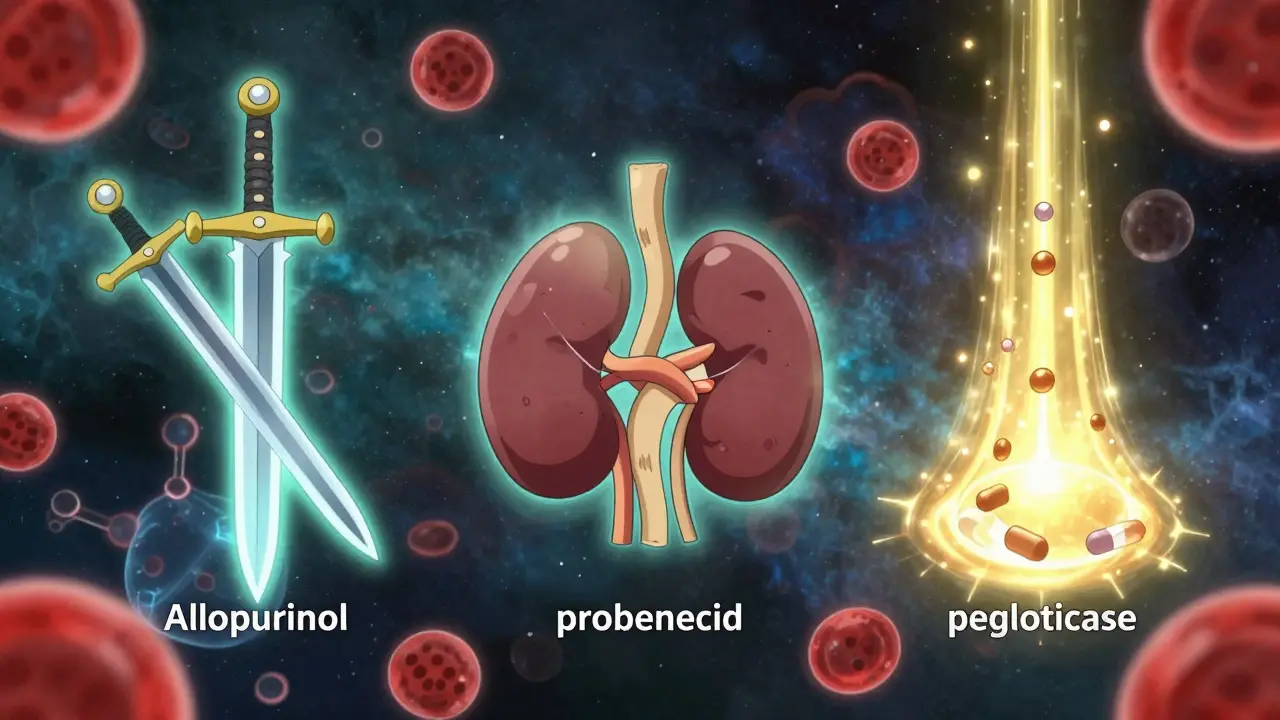
How Do Urate-Lowering Medications Work?
There are three main types of drugs used to lower uric acid, and each works differently.
1. Xanthine Oxidase Inhibitors (XOIs): Stop Production
These are the first-line drugs for almost everyone. They block the enzyme xanthine oxidase, which turns purines into uric acid. Allopurinol has been around since 1966. It’s cheap-generic versions cost just $4.27 a month. But most people don’t take enough. Doctors often start at 100 mg a day, but that’s usually too low. The real key? Dose escalation. Studies show that 92% of patients reach their target uric acid level when allopurinol is slowly increased to 300 mg or more. The problem? Many doctors stop at 200 mg because they’re afraid of side effects. But for most people, that’s not enough.
Febuxostat is the newer option, approved in 2009. It’s stronger than allopurinol at lower doses. At 80 mg a day, it hits target levels in 67% of patients. But it comes with a black box warning from the FDA. A major study found it increases the risk of heart-related death compared to allopurinol, especially if you already have heart disease. So it’s not for everyone.
2. Uricosurics: Help Your Kidneys Flush It Out
These drugs block the transporters in your kidneys that suck uric acid back in. Probenecid is the oldest, approved in 1949. It works well if your kidneys are healthy and you’re not dehydrated. But if your kidney function drops below 50 mL/min, it’s useless-and risky. Lesinurad was approved in 2015, but pulled off the market in 2019 because it caused serious kidney damage. Newer drugs like verinurad are now in late-stage trials and may offer safer alternatives soon.
3. Uricase Agents: Break It Down Completely
Pegloticase is a biologic drug that turns uric acid into allantoin, a substance your body can easily remove. It’s powerful. In clinical trials, 42% of patients with severe, long-standing gout saw their tophi disappear. But it’s not simple. It’s given as an IV infusion every two weeks, costs over $16,000 a month, and triggers allergic reactions in 26% of patients. Before starting, you need to be tested for HLA-B*58:01-a genetic marker that makes severe reactions more likely. It’s a last-resort option, reserved for people who’ve failed every other treatment.
What About Diet? Can You Just Eat Your Way Out of Gout?
Yes, diet matters-but not as much as you think. Foods like liver, anchovies, sardines, and beer are high in purines. Eating them can raise your uric acid by 1-2 mg/dL. But that’s not enough to cause gout on its own. Most people with gout still have high levels even if they cut out all high-purine foods. That’s because your body makes most of the uric acid. So while avoiding organ meats and binge-drinking beer helps, it’s not a cure. Diet is support, not treatment.
The Biggest Mistake: Stopping Medication Too Soon
Here’s the truth most doctors don’t tell you: gout medication is not a short-term fix. It’s lifelong. And the moment you stop, uric acid rises again. The Gout & Uric Acid Education Society found that 61% of patients quit their meds within a year. Why? Because they feel fine. But gout doesn’t go away just because the pain does. Crystals are still there, slowly damaging your joints. The pain returns-and worse. Many patients report having more flares after stopping meds than before they started.
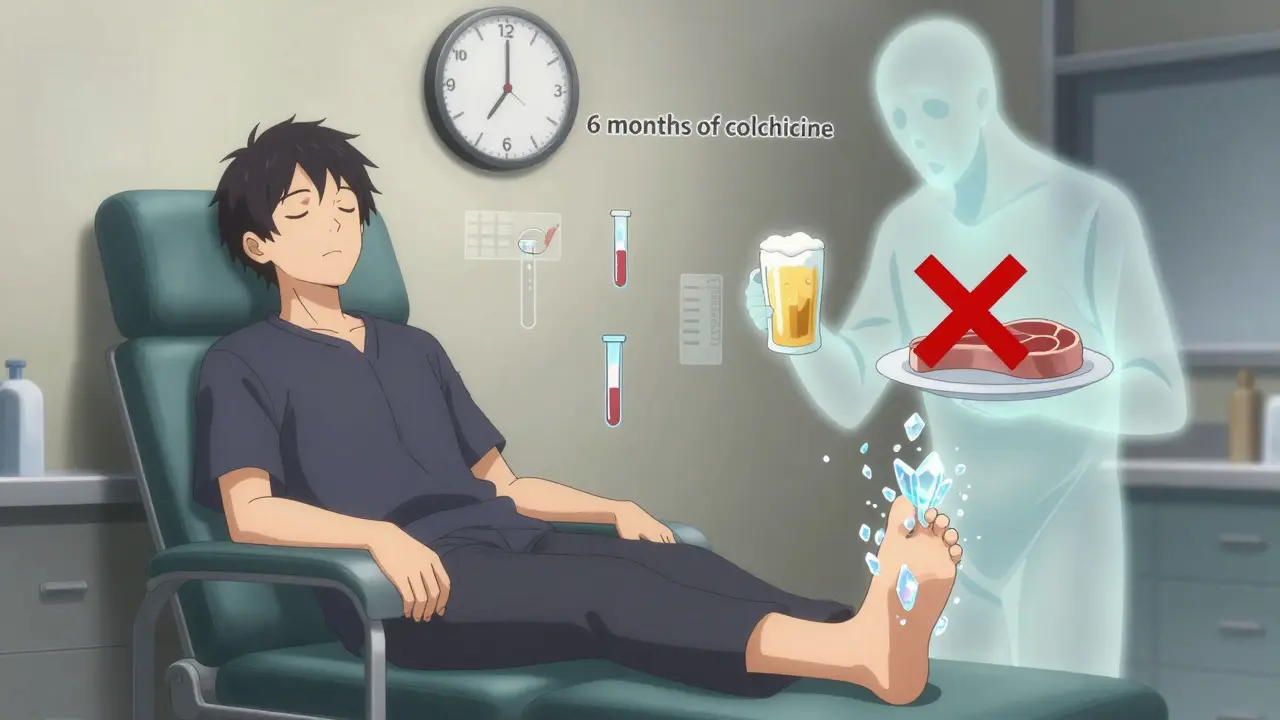
And here’s another surprise: starting urate-lowering therapy can actually trigger flares. That’s because as crystals begin to dissolve, they stir up inflammation. That’s why doctors prescribe colchicine alongside allopurinol or febuxostat for at least six months. It’s not a mistake-it’s part of the plan.
Who Gets Left Behind?
Cost is a huge barrier. Allopurinol is affordable. Febuxostat? $59 a month. Pegloticase? Over $16,000. Many patients spend months fighting insurance for approval. One Reddit user said they needed 17 prior authorizations just to get pegloticase. Meanwhile, only 37% of gout patients in the U.S. ever reach their target uric acid level. Most primary care doctors don’t monitor levels regularly. One study found only 29% check uric acid every 2-5 weeks during dose titration. That means most people are on the wrong dose, for too long, without knowing it.
What’s Coming Next?
The future of gout treatment is getting more precise. Researchers are testing drugs like arhalofenate, which lowers uric acid AND reduces inflammation. Others are looking at genetic markers-like SLC2A9 variants-that tell us who will respond best to which drug. Longer-acting uricase injections are in development. The goal? Personalized treatment. No more trial and error. Just the right drug, at the right dose, for your body.
But until then, the best advice remains simple: get your uric acid tested. If you’ve had a gout flare, ask for a uric acid blood test. If it’s above 6.8 mg/dL, talk to your doctor about starting a urate-lowering medication. Don’t wait for the next attack. Don’t assume diet alone will fix it. And don’t stop your meds just because you feel better. Gout is a chronic disease. It needs chronic management.
Key Takeaways
- Gout is caused by uric acid crystals forming in joints due to high blood levels-hyperuricemia.
- Uric acid comes mostly from your body’s own cells, not just your diet.
- Target uric acid level for most patients: below 6.0 mg/dL. For severe cases: below 5.0 mg/dL.
- Allopurinol is the first-line treatment, but most people need at least 300 mg/day to work.
- Febuxostat is more effective but carries a heart risk; avoid if you have cardiovascular disease.
- Pegloticase works for severe gout but is extremely expensive and requires careful monitoring.
- Stopping medication is the #1 reason gout comes back worse.
- Diet helps, but it’s not enough. Medication is essential for long-term control.
Can gout be cured with diet alone?
No. While avoiding high-purine foods like organ meats, shellfish, and beer can lower uric acid by 1-2 mg/dL, most people still have levels above the danger zone (6.8 mg/dL). That’s because your body makes 80% of the uric acid. Diet is helpful as a supplement, but it won’t prevent flares or dissolve crystals without medication.
Why do I still get flares after starting allopurinol?
That’s normal. When uric acid levels drop, crystals begin to dissolve, which triggers inflammation. This is why doctors prescribe colchicine along with allopurinol for at least 6 months. The flares usually stop once your uric acid stays below 6.0 mg/dL for 3 months straight. Don’t stop your meds-this is part of the healing process.
Is febuxostat safer than allopurinol?
Not for everyone. Febuxostat lowers uric acid more effectively, but the FDA issued a black box warning after a study showed it increases the risk of heart-related death compared to allopurinol. It’s only recommended for people who can’t tolerate allopurinol or have severe kidney disease (eGFR below 30). If you have heart disease, avoid it.
How often should my uric acid be checked?
When you start or adjust your medication, check every 2-5 weeks until your level is below 6.0 mg/dL. Once you’re stable, check every 6 months. Yet only 29% of primary care doctors follow this. Ask for your numbers-don’t wait for your doctor to bring it up.
What happens if I stop taking my gout medication?
Your uric acid will rise again, usually within weeks. Crystals will start to rebuild in your joints, leading to more frequent and more severe flares. Over time, this causes permanent joint damage and tophi (visible lumps under the skin). Stopping medication is the most common reason gout gets worse-not skipping beer or steak.
Are there new gout drugs coming soon?
Yes. Verinurad, a new uricosuric drug, is in Phase III trials and shows promise when combined with febuxostat, hitting target levels in 74% of patients. Arhalofenate, which lowers uric acid and reduces inflammation, is also showing strong results. Researchers are also developing longer-acting uricase injections and testing genetic markers to predict which drug will work best for you.
Kacey Yates
January 29, 2026 AT 23:44Keith Oliver
January 30, 2026 AT 00:33ryan Sifontes
January 30, 2026 AT 21:19Laura Arnal
February 1, 2026 AT 01:56DHARMAN CHELLANI
February 2, 2026 AT 13:45Jasneet Minhas
February 3, 2026 AT 06:22Alex Flores Gomez
February 3, 2026 AT 12:56Frank Declemij
February 4, 2026 AT 07:04Sheryl Dhlamini
February 4, 2026 AT 15:23Pawan Kumar
February 6, 2026 AT 12:10Eli In
February 7, 2026 AT 10:00kabir das
February 7, 2026 AT 15:48