Gluten Sensitivity Symptom Checker
Answer the following questions about your post-meal symptoms to get an initial assessment of possible gluten sensitivity:
Complete the assessment to see your results
Ever feel like your stomach swells like a balloon right after lunch and wonder if it’s the bread, pasta, or something hidden in the meal? You’re not alone. Many people blame stress, overeating, or carbonated drinks, but a growing body of evidence points to a specific trigger: gluten sensitivity. Understanding how this condition works, how it differs from celiac disease or wheat allergy, and what you can do to calm that uncomfortable puffiness can change the way you eat for the better.
What is Gluten Sensitivity?
Gluten sensitivity is a condition where the body reacts negatively to gluten - the protein mix found in wheat, barley, and rye - without the autoimmune damage seen in celiac disease. It’s also called non‑celiac gluten sensitivity (NCGS). People with gluten sensitivity often experience digestive upset, fatigue, headache, or joint pain after consuming gluten‑containing foods, yet standard blood tests for celiac disease come back normal.
The exact mechanism remains under study, but most researchers agree that a combination of innate immune activation, altered gut permeability, and changes in the gut microbiome play a role.
How Does Bloating Occur After a Meal?
Bloating is the sensation of fullness, tightness, or visible distension in the abdomen. After you eat, the stomach releases enzymes and acids to break down food, then pushes partially digested material into the small intestine. If any step falters - for example, if a protein isn’t fully broken down - gas can build up, causing that uncomfortable balloon feeling.
Key players in the bloating process include:
- Bloating itself, a symptom rather than a disease.
- The gut microbiome, a community of trillions of bacteria that ferment undigested carbs and proteins into gas.
- Digestive enzymes such as proteases and amylases that help break down proteins and carbohydrates.
- Motility of the intestines - how quickly food moves along.
When any of these factors go off‑track, gas accumulates, and you feel bloated.
Gluten Sensitivity vs. Celiac Disease vs. Wheat Allergy vs. FODMAP Intolerance
It’s easy to mix up the four conditions that often cause post‑meal discomfort. Below is a quick visual comparison.
| Condition | Immune Response | Diagnostic Markers | Typical Symptoms | Management |
|---|---|---|---|---|
| Gluten sensitivity | Innate immune activation, no antibodies | Negative celiac serology, symptom‑based | Bloating, fatigue, headache, joint pain | Gluten‑free diet, symptom monitoring |
| Celiac disease | Adaptive immune - anti‑tTG, EMA antibodies | Positive serology, intestinal biopsy | Severe bloating, diarrhea, weight loss, anemia | Strict gluten‑free diet, medical follow‑up |
| Wheat allergy | IgE‑mediated allergic reaction | Skin prick test or specific IgE | Hives, swelling, anaphylaxis, sometimes GI upset | Avoid wheat, carry epinephrine if severe |
| FODMAP intolerance | Fermentation of poorly absorbed carbs | Breath test, symptom diary after low‑FODMAP trial | Bloating, gas, abdominal pain, diarrhea | Low‑FODMAP diet, re‑introduction phase |
Notice how only celiac disease shows specific antibodies, while gluten sensitivity relies on symptom patterns. Wheat allergy is an allergic reaction that can cause life‑threatening symptoms, so it’s crucial to differentiate it from the milder gluten sensitivity.
Why Gluten Can Trigger Bloating
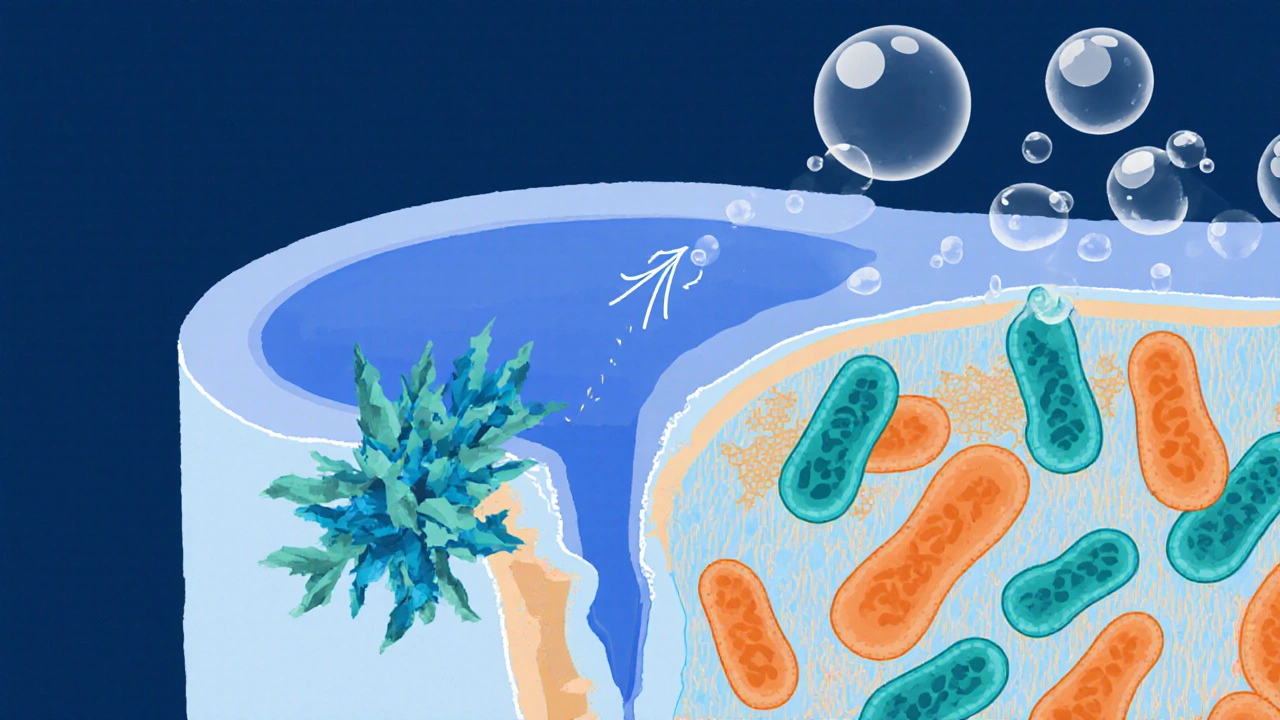
When gluten reaches the small intestine, three main things can go wrong for sensitive individuals:
- Incomplete Digestion: Gluten’s prolamin proteins are tough to break down. If protease activity is low, larger peptide fragments stay intact, providing extra fuel for gas‑producing bacteria.
- Increased Intestinal Permeability: Also called “leaky gut,” this lets gluten peptides slip through the lining, prompting an innate immune response that releases cytokines. The resulting inflammation can slow motility, trapping gas.
- Microbiome Shift: Certain bacterial strains thrive on undigested gluten peptides, producing hydrogen and methane - the gases that cause visible bloating.
Researchers at the University of Chicago (2023) measured breath hydrogen in 42 participants with self‑reported gluten sensitivity and found a 30% rise three hours after a gluten‑rich test meal, even when celiac markers were negative. This supports the idea that gluten itself can fuel gas‑producing microbes.
Identifying the Connection in Your Own Body
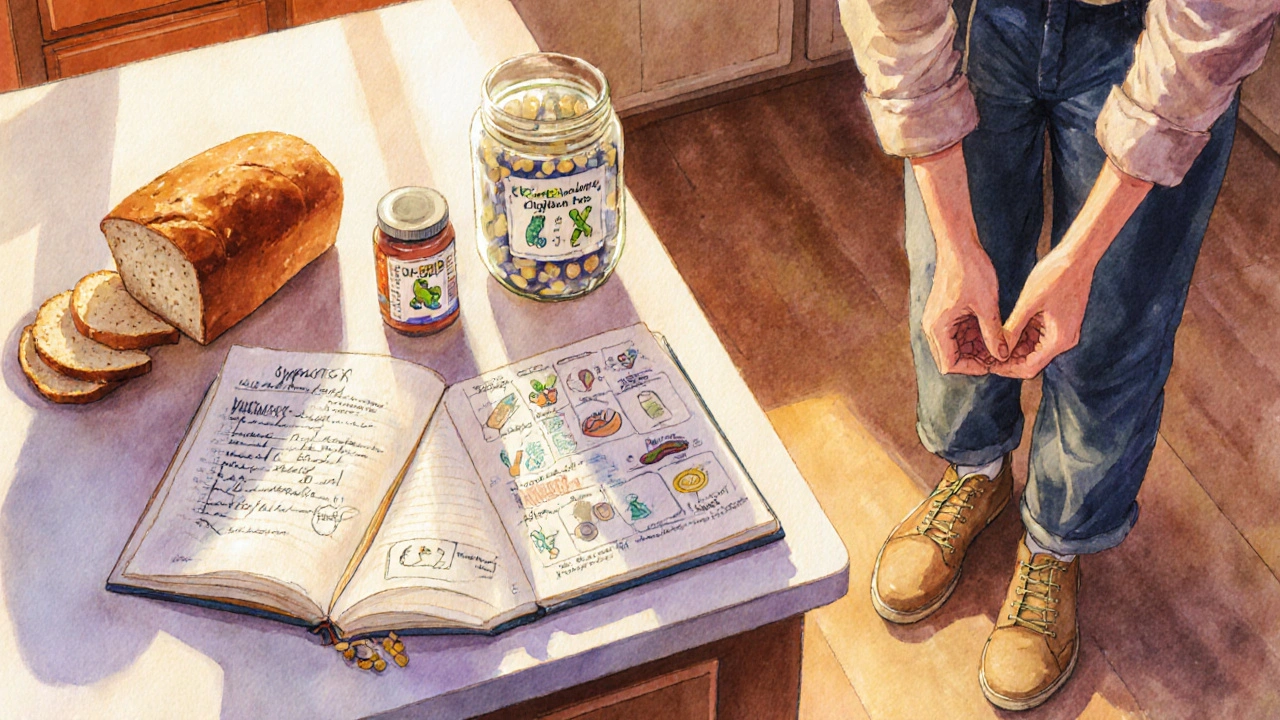
If you suspect gluten is behind your post‑meal puffiness, follow these practical steps:
- Symptom Log: Write down everything you eat for two weeks and note the timing of bloating. Look for a pattern of symptoms within 30minutes to 3hours after gluten‑containing foods.
- Elimination Trial: Remove all gluten sources (wheat, barley, rye, spelt, kamut) for 3weeks. If bloating eases, re‑introduce a controlled amount of gluten (e.g., a slice of bread) and watch for symptom return.
- Rule Out Other Causes: Consider SIBO (small intestinal bacterial overgrowth) or high‑FODMAP foods. A lactulose breath test can clarify SIBO, while a low‑FODMAP trial can separate fermentable carbs from gluten.
- Medical Testing: Get celiac serology (tTG‑IgA) and, if you’re IgA deficient, total IgA levels. Even if results are negative, a gastroenterologist can order an endoscopy if symptoms are severe.
These steps give you a clear picture without costly procedures.
Managing Bloating When Gluten Sensitivity is Present
Once you’ve confirmed a link, the goal is to keep your gut happy while still enjoying meals.
- Adopt a Gluten‑Reduced Diet: You don’t always need a 100% gluten‑free lifestyle. Many people find that limiting wheat‑based breads and pasta while allowing naturally gluten‑free grains (rice, quinoa, millet) reduces bloating enough.
- Boost Digestive Enzymes: Over‑the‑counter protease blends (e.g., lactase‑free, gluten‑digest) can help break down residual gluten peptides. Take them right before gluten‑containing meals.
- Support the Microbiome: Probiotic strains such as Bifidobacterium lactis and Lactobacillus plantarum have shown efficacy in reducing gas production. Pair probiotics with a prebiotic‑rich diet (asparagus, bananas) to maintain balance.
- Mind Fiber Types: Soluble fiber (oats, chia) can actually soothe bloating, while excess insoluble fiber from whole‑grain wheat may aggravate it. Choose gluten‑free soluble sources.
- Stay Hydrated and Move: Light walking after meals promotes transit and helps expel trapped gas.
Remember, the gut is adaptable. Small, consistent changes often yield better results than an all‑or‑nothing overhaul.
Pitfalls and Common Mistakes
Even with the best intentions, people stumble on a few frequent errors:
- Blaming Gluten for All Gas: Carbonated drinks, chewing gum, and swallowing air can add significant gas. Track these habits alongside food.
- Ignoring Hidden Gluten: Sauces, soups, and even “gluten‑free” labels can contain maltodextrin or hydrolyzed wheat protein. Reading ingredient lists is vital.
- Skipping a Full Elimination: Cutting gluten for only a few days often isn’t enough for the gut to reset. Aim for at least three weeks for a reliable assessment.
- Self‑Diagnosing Without Tests: While many manage by diet alone, severe or persistent symptoms merit professional evaluation to rule out celiac disease or other disorders.
Quick Checklist for a Gluten‑Sensitive Lifestyle
- Log meals and bloating episodes for two weeks.
- Eliminate all gluten sources for 21days.
- Re‑introduce a measured gluten portion and monitor symptoms.
- Consider a breath test for SIBO if bloating persists.
- Choose gluten‑free whole grains, boost enzymes, and add supportive probiotics.
Frequently Asked Questions
Can I have occasional gluten and still avoid bloating?
Many with gluten sensitivity find a low‑gluten approach works - for example, limiting wheat to once a week and pairing it with enzyme supplements can keep symptoms at bay. Consistency is key; the gut needs time to recover after each exposure.
How is gluten sensitivity diagnosed without a blood test?
Diagnosis is primarily clinical: a documented symptom pattern, a negative celiac work‑up, and a positive response to a gluten‑elimination/re‑introduction protocol. Some clinicians also use certified questionnaires like the Salerno criteria.
Is a gluten‑free diet healthier than a regular diet?
Not necessarily. Gluten‑free processed foods can be low in fiber and high in sugar. For non‑sensitive people, whole‑grain wheat provides valuable nutrients. Focus on naturally gluten‑free whole foods rather than relying on packaged "gluten‑free" snacks.
Could my bloating be caused by something other than gluten?
Absolutely. High‑FODMAP foods, lactose intolerance, SIBO, and even stress can all produce similar symptoms. A systematic approach - eliminating one variable at a time - helps pinpoint the true culprit.

Gabe Crisp
October 6, 2025 AT 12:10Avoiding gluten without testing is a dangerous personal choice that fuels the hidden agenda of the food lobby.
Paul Bedrule
October 16, 2025 AT 23:22When we interrogate the etiological nexus between post‑prandial distension and gluten exposure, we must first delineate the phenomenological substrate of non‑celiac gluten sensitivity (NCGS). The ontological status of NCGS resides at the interstice of innate immune activation and dysregulated microbiota‑derived metabolomics. Empirical data from controlled gluten challenges reveal a statistically significant elevation in exhaled hydrogen, signifying microbial fermentation of incompletely hydrolyzed gliadin peptides. This biochemical cascade precipitates a perturbation of the enteric nervous system, augmenting visceral hypersensitivity and motility dysrhythmia. Moreover, the permeability of the intestinal epithelium, colloquially termed “leaky gut,” is modulated by zonulin release secondary to gluten‑induced tight‑junction disassembly. The resultant translocation of antigenic epitopes catalyzes a localized cytokine milieu, predominantly interleukin‑8 and tumor necrosis factor‑α, which perpetuates low‑grade inflammation. From a systems‑theoretic perspective, the gut‑brain axis transduces these peripheral signals into central somatic awareness, manifesting as bloating, fatigue, and cranial pressure. It is imperative to appreciate the bidirectional feedback loop wherein psychosomatic stress amplifies gut dysbiosis, thereby exacerbating symptomatology. Clinical praxis therefore mandates a bifurcated diagnostic algorithm: exclusion of celiac serology followed by an empiric gluten elimination protocol. Quantitative symptom scoring before and after the elimination phase furnishes a robust inferential substrate for causal attribution. In the event of residual bloating, differential considerations such as small intestinal bacterial overgrowth or fermentable oligo‑di‑mono‑saccharides (FODMAPs) must be systematically investigated. Nutritional genomics further suggests polymorphisms in the HLA‑DQ2/DQ8 haplotype may predispose to heightened immunogenicity, albeit without overt serological markers. Ultimately, the clinician’s epistemic humility is essential, acknowledging that the mechanistic tapestry remains partially obscured. Future translational research should prioritize metagenomic profiling to elucidate the microbial consortia that thrive on gluten‑derived substrates. By integrating molecular, immunological, and psychosocial dimensions, we approach a holistic ontology of gluten‑related post‑meal bloating.
yash Soni
October 27, 2025 AT 09:34You think gluten is the villain. Sure, that’s why the whole world was waiting for a gluten apocalypse.
Emily Jozefowicz
November 6, 2025 AT 20:46Oh, the drama of blaming wheat for every rumble in the belly is truly Oscar‑worthy. While we applaud the theatrical flair, the science tells us that not every bubble is a gluten ghost. A measured approach with a dash of humor often yields clearer insights than a full‑blown culinary conspiracy.
Franklin Romanowski
November 17, 2025 AT 07:58I hear the frustration that comes with unpredictable post‑meal swelling, and that feeling can be genuinely draining. A gentle log of meals and symptoms can illuminate patterns that feel invisible at first glance.
Brett Coombs
November 27, 2025 AT 19:10They don’t want you to know that the big grain corporations are pumping secret additives to keep us hooked. It’s all part of the hidden agenda they hide behind “health foods”.
John Hoffmann
December 8, 2025 AT 06:22The distinction between gluten‑induced bloating and other gastrointestinal disturbances is clinically significant. Accurate documentation of symptom onset, frequency, and severity provides the foundation for differential diagnosis. Consequently, physicians can tailor investigative pathways with precision.
Shane matthews
December 18, 2025 AT 17:34Keeping a simple food diary helps track triggers and see if gluten really is the culprit
Rushikesh Mhetre
December 29, 2025 AT 04:46Give it a go!!! Eliminate gluten for three weeks and watch the belly balloon deflate!!! You’ll thank yourself later!!!
Sharath Babu Srinivas
January 8, 2026 AT 15:58Documenting your meals alongside symptom scores enhances data reliability 😊. This method aligns with evidence‑based practice and facilitates constructive discussions with healthcare providers.
Halid A.
January 19, 2026 AT 03:10It is advisable to verify serological markers for celiac disease prior to initiating a gluten‑free trial, thereby ensuring comprehensive diagnostic coverage. Subsequent elimination and re‑challenge phases can then be performed with methodological rigor.
Brandon Burt
January 29, 2026 AT 14:22Honestly, the whole “gluten is the evil mastermind behind every post‑meal puffiness” narrative feels overblown, especially when you consider the myriad of other dietary culprits that lurk behind the scenes, from hidden FODMAPs to carbonated beverages, and let’s not forget the psychological impact of stress eating; while the article provides a solid overview, it could have benefitted from a deeper dive into the methodological limitations of self‑reported symptom surveys, the role of placebo effects, and the nuanced differences between innate immune activation and adaptive autoimmunity; in essence, presenting gluten as the singular villain oversimplifies a complex physiological tapestry and may inadvertently steer readers toward unnecessary dietary restrictions.
Gloria Reyes Najera
February 9, 2026 AT 01:34i cant believe ppl still think gluten is the only problem its not even the biggest issue just another fad
Gauri Omar
February 19, 2026 AT 12:46The drama of blaming gluten for every belly ache is exhausting, yet some folks cling to it like a lifeline in a storm, refusing to see the broader picture.
Willy garcia
March 1, 2026 AT 23:58Tracking patterns can reveal hidden triggers and empower you to make informed choices