Every year in the U.S., about 2 million fractures happen because of weak bones. Most of these aren’t from car crashes or sports injuries-they’re from simple falls, like slipping on a rug or stumbling on a step. These are called fragility fractures, and they mostly affect people over 50. The good news? Many of them are preventable. The key lies in understanding the real role of calcium, vitamin D, and bone-building medications-and what actually works, based on solid science.
Calcium and Vitamin D: What the Evidence Really Says
For decades, doctors told everyone to take calcium and vitamin D supplements to protect bones. But the science has shifted. A major 2019 review in JAMA Network Open looked at data from over 49,000 people in six studies. It found that taking 800-1,000 IU of vitamin D3 daily with 1,000-1,200 mg of calcium reduced hip fractures by 16% and any fracture by 6%. That sounds promising, right? But here’s the catch: this only worked in people who were truly deficient.
When researchers looked at people taking just 400 IU of vitamin D and 1,000 mg of calcium-the common dose in over-the-counter pills-they found no benefit at all. The Women’s Health Initiative trial, which followed 36,000 postmenopausal women, showed zero reduction in hip or total fractures with this low-dose combo. That’s why the U.S. Preventive Services Task Force (USPSTF) now says: Don’t take low-dose calcium and vitamin D supplements if you’re healthy and living at home. It doesn’t help, and it might even hurt.
Why? Because if your body already has enough vitamin D, more won’t strengthen your bones. And too much calcium? It can raise your risk of kidney stones. The same study found a 17% higher chance of developing them. There’s also evidence that high-dose calcium (over 1,000 mg/day) may slightly increase heart attack risk, according to the FDA’s 2021 warning.
So who actually benefits? People with low vitamin D levels (below 20 ng/mL), those with poor calcium intake (less than 700 mg/day), and especially older adults living in nursing homes. The landmark 1992 Chapuy trial showed a 43% drop in hip fractures among nursing home residents who got 800 IU of vitamin D and 1,200 mg of calcium. Their average vitamin D level was only 12.3 ng/mL-severely deficient. When researchers repeated this in community-dwelling seniors with levels around 18.5 ng/mL, the benefit vanished. Context matters.
When Supplements Alone Aren’t Enough
If you’ve already broken a bone-or if your bone density scan shows osteoporosis-calcium and vitamin D alone won’t cut it. You need stronger tools. That’s where bone-building medications come in.
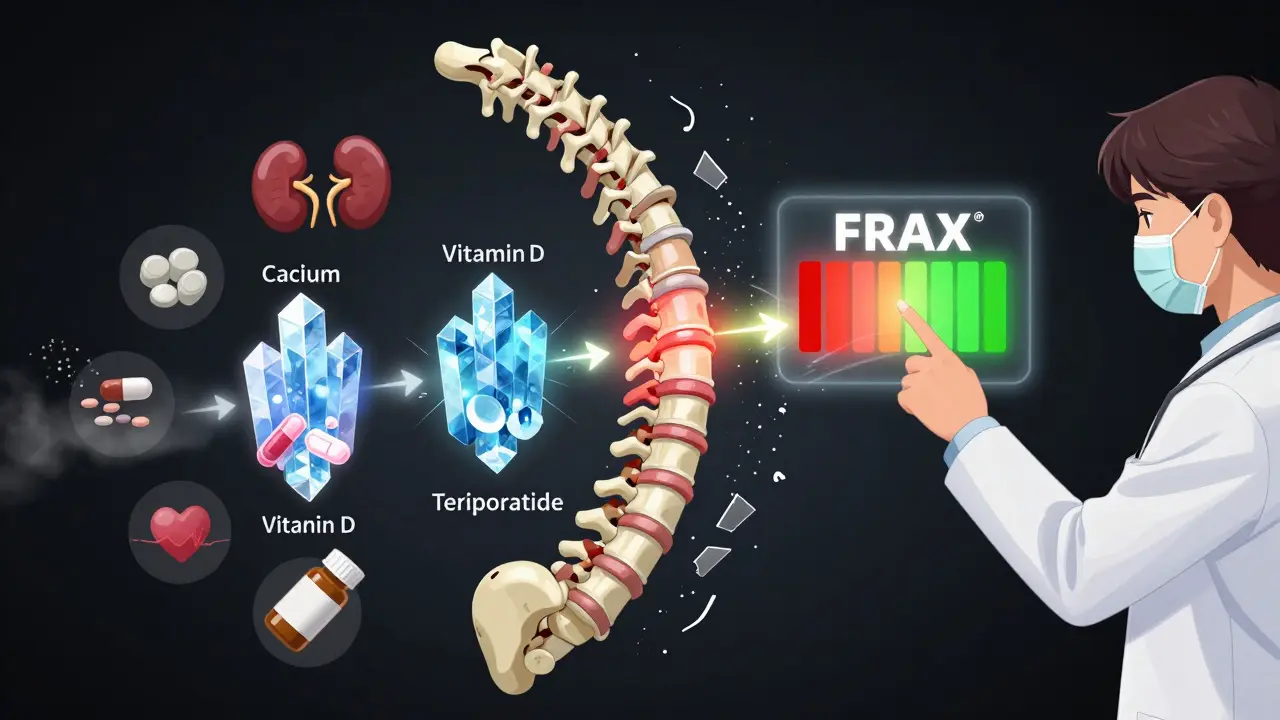
There are two main types: antiresorptives (which slow bone loss) and anabolics (which build new bone). Bisphosphonates like alendronate (Fosamax) and zoledronic acid (Reclast) are the most common antiresorptives. The Fracture Intervention Trial (FIT) showed alendronate reduces spine fractures by 44% and hip fractures by 20-50%. Zoledronic acid, given as a yearly IV infusion, cuts hip fractures by 41% over 18 months. These aren’t small gains-they’re life-changing.
But they’re not perfect. About 68% of people taking oral bisphosphonates report stomach upset, nausea, or heartburn. A quarter of them quit within a year because of side effects. That’s a huge problem. If you don’t take the medicine, it doesn’t work. That’s why some doctors now prefer injectable options like zoledronic acid or denosumab (Prolia), which only need to be given every six months.
Anabolic drugs like teriparatide (Forteo) and romosozumab (Evenity) are newer. They don’t just slow bone loss-they actually rebuild it. Teriparatide, given as a daily injection, can increase spine bone density by 9-13% in a year. The 2021 DATA-Switch trial showed that starting with teriparatide and then switching to an antiresorptive cut new spine fractures by 73% more than bisphosphonates alone. That’s a game-changer for people with severe osteoporosis.
But these drugs come with risks. Bisphosphonates can rarely cause atypical femur fractures (about 1 in 1,000 after 5 years) or osteonecrosis of the jaw (about 1 in 10,000). That’s why dentists now check your oral health before you start these meds. And you can’t take zoledronic acid if your kidney function is below 35 mL/min.
Who Needs What? A Practical Guide
Not everyone needs the same thing. Here’s how to think about it:
- If you’re healthy, over 50, and living independently: Skip the supplements. Eat calcium-rich foods (dairy, leafy greens, sardines), get sunlight, and stay active. No need to pop pills unless your blood test shows deficiency.
- If you’re deficient in vitamin D (below 20 ng/mL): Get tested. If low, take 50,000 IU of vitamin D2 weekly for 8-12 weeks, then switch to 800-2,000 IU daily. Pair it with 1,000-1,200 mg of calcium.
- If you’ve had a fragility fracture or have osteoporosis: Talk to your doctor. You likely need a prescription medication. Start with a bisphosphonate unless you’re at very high risk-then consider an anabolic agent.
- If you can’t tolerate oral meds: Ask about denosumab (Prolia) injections every 6 months or zoledronic acid once a year.
The Fracture Risk Assessment Tool (FRAX®) helps doctors decide. It uses your age, sex, bone density, and history of fractures to calculate your 10-year risk. In the U.S., if your risk of major fracture is over 20%, treatment is recommended. In the UK, it’s 15%. This isn’t guesswork-it’s precision medicine.
Why So Many People Are Taking the Wrong Stuff
Here’s the uncomfortable truth: most people are taking supplements they don’t need. A 2022 study found 35% of U.S. adults over 50 take vitamin D-and 18% are taking more than the 4,000 IU daily upper limit. Why? Because it’s easy. It’s marketed as a “bone health miracle.” But science says otherwise.
Doctors still prescribe low-dose supplements because patients demand them. At a 2022 bone health conference, 40% of primary care doctors admitted they kept prescribing them despite guidelines. One Reddit user wrote: “My mom refuses calcium because it gives her constipation.” Another said: “Patients think vitamin D is a cure-all-but they stop after three months.” Compliance is the silent killer of treatment success.
And the cost? It’s not just money. It’s risk. Unnecessary supplements can lead to kidney stones, heart issues, or false confidence. You might think you’re protecting yourself, but you could be doing more harm than good.
What’s Next? New Treatments and Big Questions
The field is evolving fast. In 2023, the FDA approved abaloparatide-SC (Tymlos) for men with osteoporosis-something only available for women before. The European Society just recommended starting with anabolic drugs for severe cases, then switching to antiresorptives. That’s a big shift from the old “start with bisphosphonates” rule.
And the big trial to watch? The VITAL-DEP study, currently enrolling 1,200 people with low vitamin D and depression. It’s testing whether 2,000 IU of vitamin D daily can prevent fractures in this high-risk group. Results come in late 2025.
But the real challenge isn’t the science-it’s the behavior. Even the best drugs fail if people don’t take them. One study found over 50% of people stop oral bisphosphonates within a year. That’s why doctors now focus on simplicity: fewer pills, fewer doses, fewer side effects. Injectable options, better patient education, and routine follow-ups are making a difference.
The bottom line? Fracture prevention isn’t about taking more pills. It’s about taking the right ones-based on your body, your history, and your risk. Calcium and vitamin D help, but only if you’re truly deficient. Medications save lives-but only if you stick with them. Talk to your doctor. Get tested. Don’t guess. Your bones will thank you.

Sarah B
February 7, 2026 AT 22:06Heather Burrows
February 8, 2026 AT 15:17Savannah Edwards
February 10, 2026 AT 13:41Gouris Patnaik
February 11, 2026 AT 03:07AMIT JINDAL
February 11, 2026 AT 22:55Amit Jain
February 13, 2026 AT 05:40Eric Knobelspiesse
February 14, 2026 AT 04:15Jesse Lord
February 15, 2026 AT 11:33Lakisha Sarbah
February 15, 2026 AT 19:58Ariel Edmisten
February 16, 2026 AT 08:53Mayank Dobhal
February 17, 2026 AT 09:35Ashley Hutchins
February 17, 2026 AT 20:43Paula Sa
February 18, 2026 AT 18:14Joey Gianvincenzi
February 20, 2026 AT 08:55