Medication mistakes are one of the leading causes of hospital visits for seniors
Every year, over 350,000 preventable drug-related emergencies happen in nursing homes and homes across the U.S. - and most of them are avoidable. Seniors take more medications than any other age group. Nearly 90% of people over 65 take at least one prescription drug, and 40% take five or more daily. Add in over-the-counter pills, vitamins, and supplements, and it’s easy to lose track. That’s where things go wrong. A missed dose. A double dose. A dangerous mix of drugs. A pill stored where a grandchild can reach it. These aren’t just mistakes - they’re risks that can end independence, hospitalize someone, or worse. The good news? Simple, practical steps can cut these risks dramatically. Here are five proven, real-world ways seniors and caregivers can keep medications safe.
Keep a live, detailed medication list - update it after every change
Don’t rely on memory. Don’t guess what’s in the medicine cabinet. Write it all down - every single thing taken, every day. That includes prescriptions, pain relievers like ibuprofen or acetaminophen, sleep aids, heartburn meds, fish oil, ginseng, magnesium, and anything else. The list needs more than just names. For each medication, record: the exact dose (e.g., 10 mg, not "one pill"), how often it’s taken (e.g., "twice daily with food"), why it was prescribed, the doctor’s name, the pharmacy phone number, and the expiration date. The Health in Aging Foundation says this list should have 10 key details. If you don’t have them all, call your pharmacy. They’ll help you build it.
Update this list within 24 hours of any change - whether a new drug was added, a dose was changed, or one was stopped. Bring this list to every doctor’s visit, ER trip, or pharmacy pickup. Pharmacists say 92% of dangerous drug interactions are caught just by seeing this list. A 78-year-old woman in Ohio missed a hospitalization because her pharmacist spotted a conflict between her new blood pressure pill and her old cholesterol drug - a mix that could have caused her heart to race dangerously. She had the list. Her doctor didn’t. That list saved her.
Use a pill organizer - but choose the right one
Pill organizers aren’t just for seniors with memory problems. They’re for anyone juggling multiple pills at different times of day. A simple 7-day organizer with AM and PM compartments cuts missed doses by nearly half, according to a 2021 study by the National Institute on Aging. But not all organizers work the same. If someone has trouble reading small print, get one with large labels. If they tend to forget if they already took a pill, use one with a locking lid. If they have dementia, avoid ones with too many compartments - 14 slots can be overwhelming. Start simple: a single-day, two-compartment box. Then move up as needed.
Some caregivers swear by digital tools like Medisafe or Hero. Medisafe sends phone alerts and lets you track if pills were taken. Hero is a smart dispenser that releases pills automatically and texts you if a dose is skipped. But tech isn’t perfect. One caregiver in Florida paid $100 for an app that her mother kept dismissing without taking pills - and she didn’t know until she had a low blood sugar episode. If the person gets confused by screens, stick with physical organizers. A laminated chart with photos of each pill next to its name and purpose helped one man reduce his anxiety by 80%. Sometimes, the simplest solution works best.
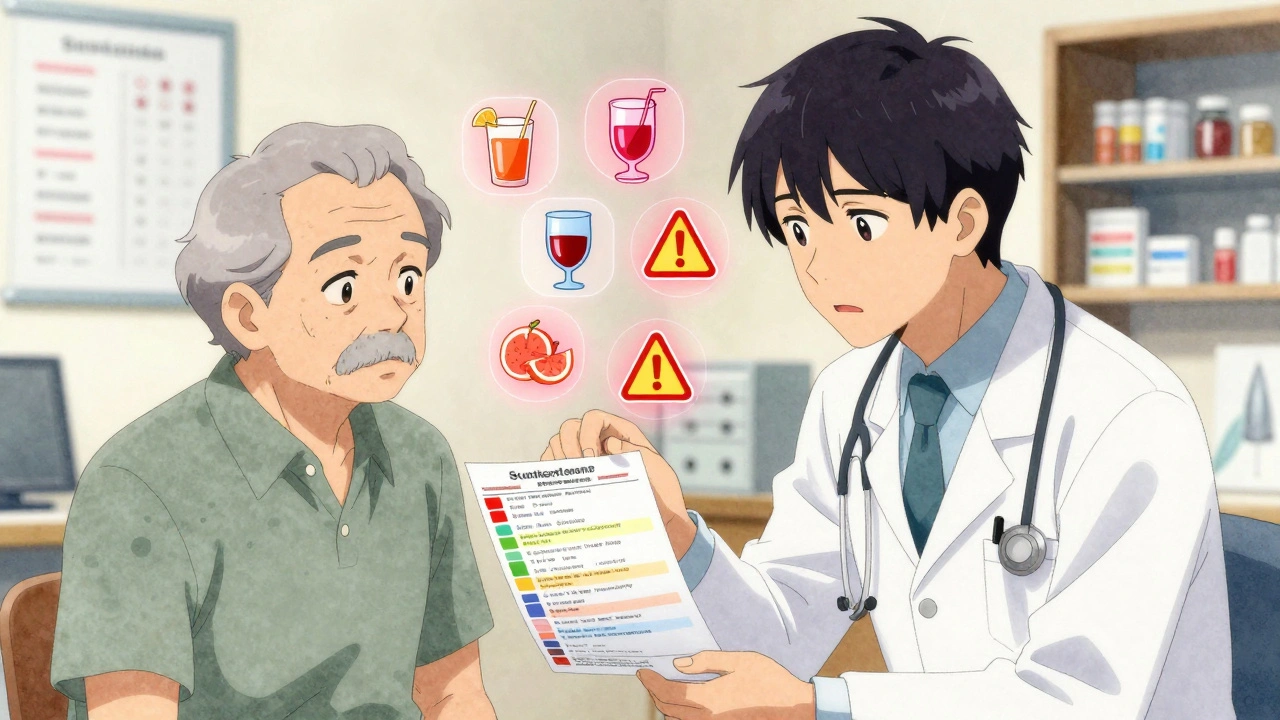
Check for drug interactions - especially with food and alcohol
It’s not just about mixing two pills. What you eat or drink can change how a drug works. Grapefruit juice is a silent danger. It interferes with 85 common medications, including statins for cholesterol and certain blood pressure drugs. One sip can make the medicine too strong - leading to muscle damage or dangerous drops in blood pressure. Alcohol is another big risk. It interacts with over 150 medications, including sleep aids, antidepressants, diabetes drugs, and painkillers. Mixing alcohol with these can cause dizziness, falls, liver damage, or even coma.
Use the Beers Criteria®, updated every two years by the American Geriatrics Society. It lists 138 medications that are risky for seniors - things like benzodiazepines for anxiety or long-term NSAIDs like ibuprofen. If a doctor prescribes something new, ask: "Is this on the Beers list?" Also, ask about interactions with any supplements. St. John’s Wort can make blood thinners useless. Calcium can block thyroid meds. Always check. A 2022 study found that 63% of medication errors in dementia patients were avoided when caregivers asked these exact questions at every appointment.
Store meds properly - and lock them away
Most seniors keep their meds in the bathroom. That’s the worst place. Heat and steam from showers degrade pills. A University of Florida study found that 37% of common medications lose effectiveness when stored in a humid bathroom. The ideal spot? A cool, dry place - like a bedroom drawer, away from windows. Temperature should stay between 68°F and 77°F. Keep all meds in their original bottles. That way, you can see the label, expiration date, and instructions.
If you have grandchildren, toddlers, or even curious teens in the house, lock the meds. The Poison Control Center reports 60,000 accidental poisonings in kids each year from unsecured medications. A locked box costs under $20 and can be found at any pharmacy. Even if you think "they’d never touch it," trust us - they will. One grandmother in Texas kept her insulin in the fridge. Her 4-year-old grandson found it, injected himself, and ended up in the ER. That’s why locking isn’t optional - it’s essential.

Talk to your doctor - ask the right questions
Doctors are busy. They don’t always know what you’re taking unless you tell them. And they don’t always realize a pill isn’t needed anymore. That’s why you need to ask five questions at every visit:
- Is this medication still necessary?
- What interactions should I watch for?
- Are there cheaper or simpler alternatives?
- What are the signs of a bad reaction?
- Can we reduce how often I take this?
Dr. Michael Steinman’s 2023 study in JAMA Internal Medicine showed that simplifying a regimen - from four times a day to once - boosts adherence from 50% to 90%. That’s huge. If you’re taking 10 pills, ask if any can be stopped. The American Geriatrics Society’s "Choosing Wisely" campaign says seniors often take drugs that do more harm than good - especially sleeping pills, antipsychotics, and long-term painkillers. Deprescribing - safely stopping unnecessary meds - reduces falls by 22% and hospital stays by 18%.
Also, ask about free help. The NIA’s "Medication Check-Up" program offers free in-home reviews by pharmacists through 11,000 Area Agencies on Aging. Medicare Part D also offers free medication therapy management for those on eight or more drugs. Use it. Don’t wait for a crisis.
Common mistakes that put seniors at risk
Even with the best intentions, people make these errors - and they’re dangerous:
- Crushing pills that are meant to be swallowed whole. Time-release meds can become overdose risks if crushed. A 2022 University of Michigan study found this happened in 22% of home care situations.
- Keeping expired meds. The average senior home has $317 worth of old, unused pills. Throw them out. Use a drug take-back program or mix them with coffee grounds and throw them in the trash - don’t flush them.
- Sharing meds. "I had this for my knee pain - take one." Never do this. A pill that helps you could hurt someone else.
- Ignoring side effects. Dizziness, confusion, nausea, or a rash aren’t "just aging." They could be signs of a bad reaction. Report them immediately.
Medication safety isn’t about perfection. It’s about consistency. One day, you forget to update the list. Another day, you skip the pill organizer. But if you make these five steps part of your routine - like brushing your teeth - you’ll prevent more problems than you can imagine. Seniors who follow these tips are far less likely to end up in the hospital. Caregivers who use them sleep better, worry less, and feel more in control. It’s not magic. It’s just smart, simple habits - and they work.
What should I do if my senior parent skips a dose?
Don’t double the next dose unless the doctor says so. Instead, call the pharmacy or prescribing doctor. Most medications have clear instructions for missed doses. If it’s been less than a few hours, take it. If it’s close to the next dose, skip it. Keep a log of missed doses - this helps doctors spot patterns. If skipping doses happens often, talk to the doctor about switching to a once-daily version or using a smart dispenser.
Can I use a smartphone app instead of a pill organizer?
Apps like Medisafe or MyTherapy can help, but they’re not for everyone. Seniors with memory issues or who don’t use phones well may get frustrated or ignore alerts. Studies show apps work best when paired with a physical organizer or caregiver check-in. If you use an app, make sure a family member gets alerts if a dose is missed. Otherwise, you might not know until it’s too late. For many, a simple pill box with large print is more reliable.
How do I know if a medication is no longer needed?
Ask your doctor or pharmacist during every visit. Many meds are prescribed for short-term use - like antibiotics after surgery or sleep aids after a hospital stay - but keep getting refilled automatically. The American Geriatrics Society recommends reviewing all meds at least once a year. If a condition has improved (like high blood pressure controlled for two years), ask if the drug can be lowered or stopped. Never stop a medication on your own. Always get professional advice.
Are generic drugs safe for seniors?
Yes. Generic drugs contain the same active ingredients as brand-name versions and are regulated by the FDA to work the same way. They’re often much cheaper - which matters for seniors on fixed incomes. Some people worry generics aren’t as strong, but that’s a myth. If you notice a change in how you feel after switching, tell your doctor. But don’t assume the generic is the problem. Sometimes, the brand-name version has different fillers that cause side effects.
What if my senior parent refuses to take their meds?
Refusal is common, especially with dementia or depression. Don’t force it. Try to understand why. Is it because of side effects? Confusion? Fear? Taste? Sometimes, changing the form helps - like switching from a pill to a liquid or patch. Ask the doctor if a different version exists. Use a consistent routine - give meds after breakfast or before bed, always in the same spot. If it’s a mental health issue, talk to the doctor about behavioral strategies or counseling. Support groups like the Alzheimer’s Association offer tips from other caregivers who’ve been there.
Next steps for caregivers and seniors
Start today. Don’t wait for a crisis. Here’s what to do right now:
- Go to the medicine cabinet. Pull out every pill, bottle, and supplement.
- Write down everything - name, dose, frequency, purpose.
- Call your pharmacy. Ask them to print a complete, updated list.
- Buy a simple 7-day AM/PM pill organizer. Get one with a lock if needed.
- Find a cool, dry spot to store meds - not the bathroom.
- Write down the five questions to ask at your next doctor visit.
Do this in one afternoon. It takes less than two hours. But it could prevent months of hospital stays, confusion, or worse. Medication safety isn’t complicated. It’s just something you have to do - regularly, carefully, and with care.
Larry Lieberman
December 8, 2025 AT 10:26Iris Carmen
December 8, 2025 AT 21:53Shubham Mathur
December 9, 2025 AT 10:53Mona Schmidt
December 9, 2025 AT 19:04Lisa Whitesel
December 11, 2025 AT 04:06Raja Herbal
December 12, 2025 AT 17:03William Umstattd
December 13, 2025 AT 20:02Andrea Beilstein
December 13, 2025 AT 20:59Guylaine Lapointe
December 14, 2025 AT 02:41Jennifer Blandford
December 14, 2025 AT 17:46