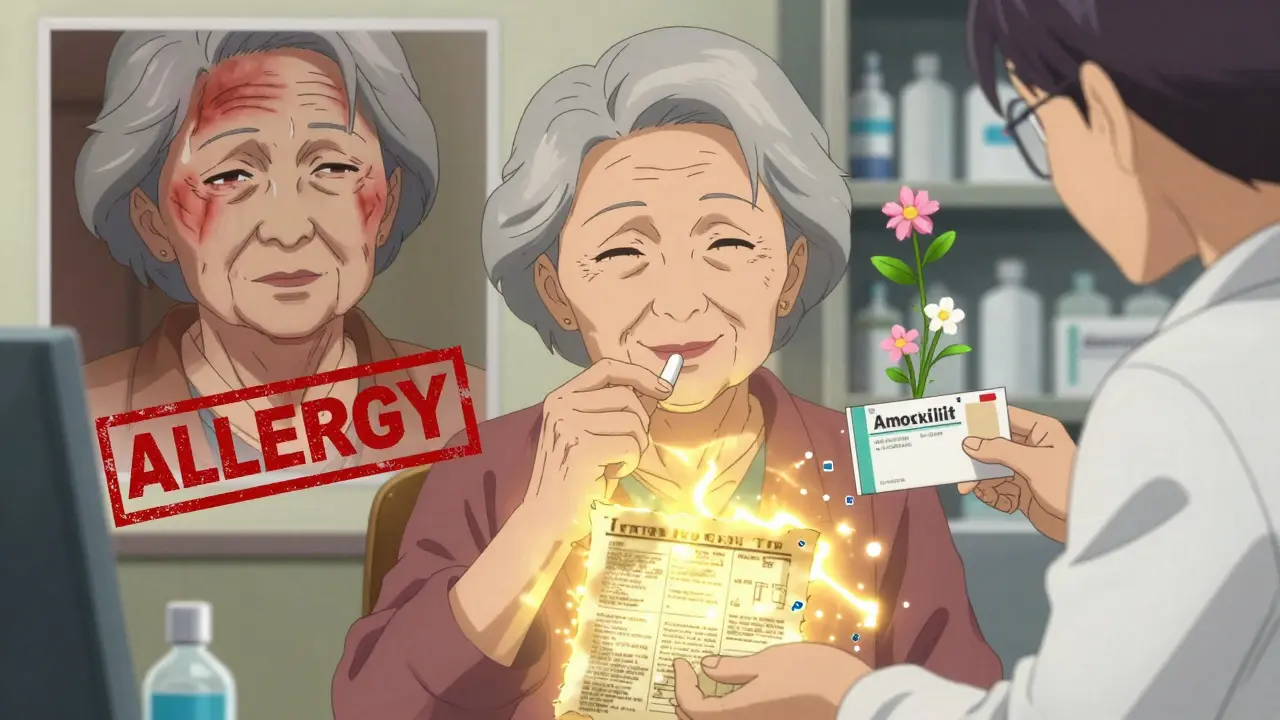
More than 10% of people in the U.S. believe they’re allergic to penicillin. But here’s the shocking truth: over 95% of them aren’t. That label-written in their chart after a childhood rash or a vague reaction decades ago-isn’t just wrong. It’s dangerous. It’s limiting your treatment options, increasing your risk of resistant infections, and costing the healthcare system billions every year.
Why a False Allergy Label Is More Than Just an Inconvenience
If you’ve been told you’re allergic to penicillin, you’ve probably been given alternatives like azithromycin, clindamycin, or fluoroquinolones. These drugs work-but they’re not better. They’re broader, harsher, and more likely to cause side effects like severe diarrhea, yeast infections, or even life-threatening C. difficile infections. The CDC estimates that false penicillin allergy labels contribute to over 50,000 extra C. diff cases each year in the U.S. alone. Doctors avoid penicillin and related antibiotics-like amoxicillin or cephalexin-because they’re afraid of triggering a reaction. But here’s what they don’t tell you: true IgE-mediated penicillin allergy (the kind that causes anaphylaxis) affects less than 1-2% of the population. The rest? Most reactions were never allergies at all. A rash from a virus? A side effect of the infection? A non-allergic skin reaction? These get mislabeled as “penicillin allergy” and stick for life.How You Got Labeled (And Why It’s Probably Wrong)
Many people get labeled allergic to penicillin after a mild rash as a child. Maybe they had a viral illness at the same time. Maybe they took the antibiotic for a sore throat that was actually strep, and the rash came from the virus-not the drug. Or maybe they had nausea or diarrhea, which are common side effects, not allergies. Allergies involve your immune system. True penicillin allergies cause hives, swelling, trouble breathing, or low blood pressure within minutes to hours. Most people who say they’re allergic never had anything like that. Yet the label stays. Why? Because no one ever tested it. No one ever asked: “What exactly happened? Was it a rash? When? Did you need epinephrine?”How Testing Works: Skin Tests, Challenges, and What to Expect
Getting tested isn’t complicated-but it’s not something your GP can do in a 10-minute visit. It requires a structured approach. Step 1: History Review - Your doctor will use a tool called PEN-FAST. It asks five simple questions:- Was the reaction 5 or more years ago?
- Was it anaphylaxis or angioedema?
- Did you need epinephrine?
- Was it treated in a hospital?
- Was there a rash only?
What Happens After You’re Cleared?
Once you’re confirmed not allergic, your medical record gets updated. Not just “penicillin allergy removed.” It’s changed to: “Penicillin allergy label removed after negative testing.” That’s important. It shows your history was reviewed, not just erased. Now, if you get pneumonia, a sinus infection, or a UTI, your doctor can prescribe the best, safest, cheapest antibiotic: amoxicillin. No need for expensive, broad-spectrum drugs. No more bloating, yeast infections, or diarrhea from clindamycin. You get better faster-with fewer side effects. One patient in Massachusetts, 68, had been labeled allergic for 40 years. She kept getting recurrent UTIs because doctors avoided penicillin. After testing, she took amoxicillin for her next infection-and didn’t get sick again for two years. She saved over $28,000 in hospital bills.Why So Few People Get Tested (And How to Change That)
You’d think this would be routine. But fewer than 40% of eligible patients ever get tested. Why?- Lack of access - You need an allergist or a trained pharmacist. In rural areas, there’s one allergist for every 500,000 people.
- Doctors don’t know how - Most GPs weren’t trained in de-labeling. They don’t know about PEN-FAST or how to arrange a challenge.
- Patient fear - People are scared to try something they’ve avoided for decades. “What if I react now?”
- System barriers - Many hospitals don’t stock the right test formulations. EHR systems don’t let you easily update allergy status.
Who Should Get Tested?
You should consider testing if:- You were told you’re allergic to penicillin as a child
- Your reaction was a rash, nausea, or diarrhea-not breathing trouble
- You’ve never had a reaction since
- You’ve had to take stronger antibiotics that gave you side effects
- You’re planning surgery or might need antibiotics in the future

What If You’re Actually Allergic?
Testing doesn’t just remove false labels. It confirms real ones. If you test positive, you’ll know for sure. You’ll avoid the drug. You’ll carry an epinephrine auto-injector. You’ll know which antibiotics to avoid. And here’s the good news: even if you’re truly allergic to penicillin, you might still be able to take other antibiotics. Cross-reactivity between penicillin and cephalosporins is often overestimated. Testing can clarify that too.What to Ask Your Doctor
Don’t wait for them to bring it up. Say this:- “I’ve been told I’m allergic to penicillin. Can we check if that’s still true?”
- “Is there a way to get tested? Do you have a protocol for de-labeling?”
- “Can you refer me to someone who does oral challenges?”
Final Thought: This Isn’t Just About Penicillin
False allergy labels aren’t limited to penicillin. They happen with sulfa drugs, NSAIDs, and even chemotherapy agents. But penicillin is the most common-and the most fixable. Getting tested isn’t a luxury. It’s a smart medical decision. It’s about using the right tool for the job. It’s about safety, cost, and effectiveness. And for most people, it’s simple, safe, and life-changing.If you’ve been avoiding penicillin for decades because of a childhood rash-don’t live with that label anymore. Get tested. You might be surprised what you’re allowed to take.

Peyton Feuer
January 3, 2026 AT 13:13i got labeled penicillin allergic when i was 7 after a rash from a cold. never had any issues since. just found out last year i was never allergic. best decision ever. no more clindamycin nightmares.
Siobhan Goggin
January 4, 2026 AT 22:57This is one of those things that should be standard care. Why are we still letting outdated labels dictate treatment? It’s not just inconvenient-it’s actively harmful.
Jay Tejada
January 5, 2026 AT 11:11so you're telling me my grandpa's 40-year-old 'allergy' was just a bad case of the flu and a doctor who didn't bother asking questions? yeah. that tracks. we've all been screwed by lazy medicine.
Allen Ye
January 7, 2026 AT 04:59There’s a deeper structural failure here. We treat medical labels like tattoos instead of dynamic clinical notes. Once inked, they’re never questioned, even when evidence contradicts them. This isn’t just about penicillin-it’s about how medicine conflates convenience with accuracy. We’ve built systems that prioritize documentation over discernment, and patients pay the price in unnecessary suffering, cost, and drug resistance. The PEN-FAST tool is a bandage on a hemorrhage. What we need is a cultural reckoning: stop accepting secondhand medical history as gospel.
mark etang
January 7, 2026 AT 15:14As a healthcare professional, I cannot stress enough the importance of this initiative. Every false penicillin label is a missed opportunity for optimal patient care. We must prioritize allergist referrals and institutional protocols to correct these errors.
josh plum
January 8, 2026 AT 20:31lol so now the medical industry wants us to trust them again? after decades of pushing pills that turn your guts to mush? next they'll say vaccines are safe and your phone doesn't track you. sure. i'll take the 25mg amoxicillin... right after i get my 5G immunity bracelet.
Brendan F. Cochran
January 9, 2026 AT 10:31they want us to just swallow a pill after 40 years? what if it's a secret government test? what if the real allergy is to capitalism and this is just another way to make us pay for 'testing'? i ain't no lab rat for big pharma.
Jason Stafford
January 9, 2026 AT 17:14EVERYONE knows the FDA hides the truth about antibiotics. This 'testing' is just a distraction while they pump more toxic drugs into our water supply. That rash you had as a kid? It was your body rejecting the glyphosate in your cereal. The 'allergy' was your immune system fighting back. Now they want you to re-expose yourself? That's not medicine-that's a death sentence disguised as science.
Justin Lowans
January 11, 2026 AT 07:09This is a profoundly important public health intervention. The systemic underutilization of penicillin de-labeling represents a significant gap in antimicrobial stewardship. I commend institutions adopting automated EHR flags and standardized protocols-this is precisely the kind of evidence-based, patient-centered reform we need to scale.
Ethan Purser
January 13, 2026 AT 00:19they don't want you to know this. they don't want you to realize how many people are being overmedicated, overcharged, and over-sickened just because nobody bothered to ask what really happened when you were six. this isn't medicine-it's a money machine. and you? you're the profit margin.
Cassie Tynan
January 13, 2026 AT 11:16so i spent 30 years avoiding penicillin because i got a rash after a virus... and now you're telling me i could've had a $5 antibiotic instead of $300 IVs? wow. thanks, healthcare. you're the real MVP.
Rory Corrigan
January 13, 2026 AT 13:46we're all just glitching through a medical system that forgot how to listen. maybe if we stopped treating patients like data points, we'd stop making mistakes like this. 🤷♂️
Stephen Craig
January 15, 2026 AT 05:18Testing works. Get it done.
Connor Hale
January 17, 2026 AT 04:04It's wild how a simple question-'What exactly happened?'-could have saved so many people so much pain. We assume the system knows best. But sometimes, the system just forgot to ask.