Calcineurin Inhibitor Side Effect Comparison Tool
Cyclosporine vs Tacrolimus Side Effects
This tool compares the most common side effects between cyclosporine and tacrolimus based on clinical data. Use this to better understand potential side effects you might experience with these medications.
Important: This is not a medical diagnosis tool. Always discuss side effects with your transplant team.
| Side Effect | Cyclosporine | Tacrolimus |
|---|---|---|
| Kidney Damage |
25-75% early 10-30% permanent |
25-75% early 10-30% permanent |
| Neurotoxicity | Not common | ~40% of users |
| Tremors | Rare | 67% of users |
| Sleep Problems | Not common | 65% of users |
| Hirsutism | 30% of users | Rare |
| Gingival Hyperplasia | 15-25% of users | Rare |
| New-Onset Diabetes | 5-15% of users | 15-30% of users |
| High Blood Pressure | 50-70% of users | 50-70% of users |
| Low Magnesium | 40-60% of users | 40-60% of users |
| High Potassium | Risk | Risk |
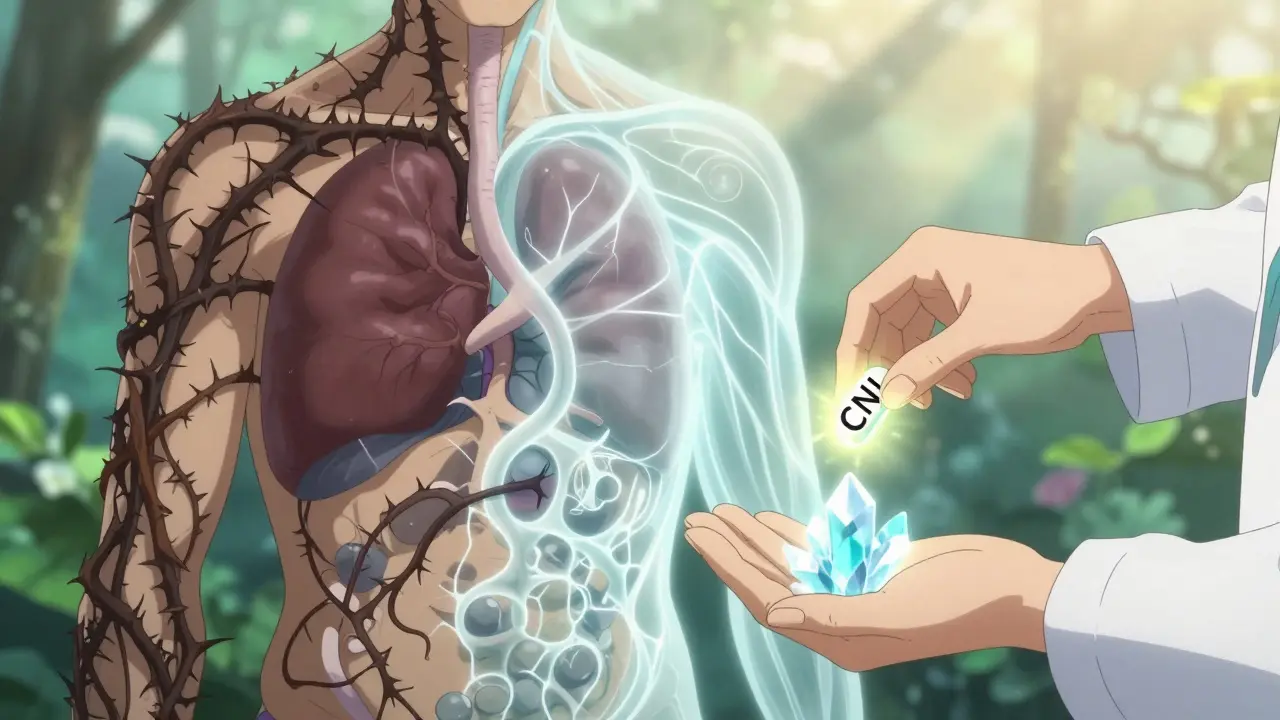
When you’ve had a kidney, liver, or heart transplant, or are being treated for a severe autoimmune disease, your doctors rely on calcineurin inhibitors like cyclosporine and tacrolimus to keep your body from rejecting the new organ or attacking itself. These drugs work by shutting down the T-cells that drive immune responses. But they don’t just stop the bad actors-they slow down your whole immune system, and that comes with a long list of side effects. For many patients, the trade-off is worth it. For others, the side effects become harder to live with than the original condition.
Why These Drugs Are Still Used Despite the Risks
Even today, nearly 90% of kidney transplant patients in the U.S. take either cyclosporine or tacrolimus. Why? Because they work. Compared to older immunosuppressants, these drugs cut acute rejection rates by more than half. A 2023 report from the Organ Procurement and Transplantation Network shows tacrolimus gives patients a 92% one-year graft survival rate, compared to 85% with cyclosporine. That difference saves lives. But survival isn’t the whole story. Many patients live for decades after transplant, and the long-term damage from these drugs can be just as serious as rejection.
The Big One: Kidney Damage
It’s ironic-these drugs are used to protect a new kidney, but they can slowly destroy it. Nephrotoxicity is the most common reason doctors have to adjust or stop these medications. About 25 to 75% of patients see their creatinine levels rise early on, which means their kidneys are struggling. That’s usually reversible if caught in time. But for 10 to 30% of long-term users, the damage becomes permanent. Scar tissue builds up in the kidney’s filtering units, leading to chronic kidney disease. A landmark 2009 study found that calcineurin inhibitors were responsible for 38% of late kidney graft failures. That’s not a small number-it’s the leading cause of transplant failure after the first year.
Tacrolimus vs. Cyclosporine: The Side Effect Battle
While both drugs cause similar problems, they each have their own signature side effects. Tacrolimus is more likely to cause tremors, trouble sleeping, and new-onset diabetes. Cyclosporine? It’s the one that makes you grow hair where you don’t want it and swells your gums.
Neurotoxicity hits nearly 40% of tacrolimus users. That means shaky hands, headaches, trouble concentrating, and in rare cases, full-blown parkinsonism. One case report from 2022 described a patient who developed severe tremors and slow movement just two weeks after starting tacrolimus. When they switched to cyclosporine, the symptoms vanished-only to come back months later. That’s not common, but it shows how sensitive the nervous system is to these drugs.
On the other hand, cyclosporine causes hirsutism in up to 30% of users-especially women. Facial hair, thickened arm hair, even dark patches on the skin. It’s not dangerous, but it’s deeply distressing. Gingival hyperplasia, or swollen gums, affects 15 to 25% of cyclosporine users. Brushing your teeth becomes painful. Some need gum surgery just to keep their mouth functional.

Diabetes Risk: Tacrolimus Takes the Lead
If you’re on tacrolimus, your risk of developing diabetes after transplant jumps to 15-30%. With cyclosporine, it’s 5-15%. Why? Tacrolimus directly interferes with insulin release from the pancreas. It blocks a signaling pathway called calcineurin-NFAT that beta cells need to respond to sugar. The result? Blood sugar spikes even if you eat normally. Many patients start needing insulin within months of starting the drug. The good news? Doctors now know to watch for early signs. If your fasting glucose starts creeping up, they may add an SGLT2 inhibitor like dapagliflozin-which doesn’t just lower blood sugar, it also protects your heart and kidneys.
High Blood Pressure, Low Magnesium, High Potassium
Almost every patient on these drugs ends up on blood pressure meds. Between 50 and 70% develop hypertension. The drugs constrict blood vessels, making the heart work harder. At the same time, magnesium levels crash in 40-60% of people. Low magnesium causes muscle cramps, irregular heartbeats, and worsens high blood pressure. Most patients need daily magnesium supplements just to stay stable.
High potassium is another silent danger. When kidneys are stressed, they can’t flush out potassium like they should. Levels above 5.0 mEq/L can trigger dangerous heart rhythms. Regular blood tests are non-negotiable. You can’t feel high potassium coming. You only find out when your ECG shows trouble-or worse.
What Patients Are Really Saying
Online patient forums tell a different story than clinical trials. On the American Transplant Foundation’s site, 68% of 1,245 people said their side effects were “moderate to severe.” The top complaints? Tremors (72%), sleep problems (65%), and managing diabetes (48%). On Reddit’s r/transplant community, cyclosporine users talk about hirsutism in 42% of posts. Tacrolimus users mention tremors in 67% of theirs. One woman wrote: “I stopped wearing sleeveless shirts because my arms looked like a man’s. I cried every time I looked in the mirror.” Another said: “I can’t hold a coffee cup without spilling. My hands shake so bad, I stopped cooking.”
A 2022 study using the Transplant Effect Questionnaire found that CNI side effects dropped quality of life scores by 15 to 22 points on a 100-point scale. That’s the difference between feeling okay and feeling broken. And here’s the kicker: 78% of patients surveyed by the National Kidney Foundation said they’d switch to a different drug if it worked just as well but didn’t wreck their body.
How Doctors Are Trying to Reduce the Damage
Doctors aren’t ignoring this. The old days of “maximum tolerated dose” are over. Now, it’s all about the “minimum effective dose.” Many centers start patients on tacrolimus at 0.1 mg/kg/day and drop it to 0.05 mg/kg within weeks if levels are stable. Trough levels are monitored weekly at first. For tacrolimus, they aim for 5-10 ng/mL. For cyclosporine, it’s 100-200 ng/mL. Stay above that, and rejection risk goes up. Go too high, and your kidneys pay the price.
Some patients are being weaned off CNIs entirely. A 2023 trial called CONVERT showed that switching to belatacept-a non-CNI drug-gave patients better kidney function and fewer metabolic problems, with the same survival rates. The NIH is now running the CIRT-T2 trial, testing whether low-risk transplant patients can stop CNIs after just three months. Early results show 89% graft survival and a 40% drop in side effects.
What You Can Do
Don’t wait for symptoms to get bad. Here’s what you should ask your team:
- Can my drug level be lowered without risking rejection?
- Am I on the lowest possible dose?
- Should I be tested for insulin resistance or early diabetes?
- Do I need magnesium or potassium supplements?
- Have you considered switching to a CNI-sparing regimen?
Track your symptoms. Keep a notebook: tremors? Sleep issues? Gum swelling? Sugar spikes? Bring it to every appointment. Your feedback helps your doctor decide if it’s time to change your plan.
The Future Is Less Toxic
Voclosporin, a newer calcineurin inhibitor approved in 2021 for lupus nephritis, causes 30% less high blood pressure than cyclosporine. That’s progress. But the real shift is moving away from CNIs altogether when possible. Belatacept, sirolimus, and other alternatives are becoming standard for patients who can’t tolerate the side effects. The goal isn’t just to keep the organ alive-it’s to keep the person healthy, too.
Can you stop taking cyclosporine or tacrolimus after a transplant?
Yes, but only under strict medical supervision. Some low-risk patients can switch to non-CNI drugs like belatacept or sirolimus after several months. This is called a CNI-sparing or CNI-withdrawal protocol. It’s not for everyone-patients with high rejection risk still need CNIs long-term. But for those with stable grafts and low immune activity, stopping CNIs can dramatically improve quality of life and protect kidney function.
Which has worse side effects: cyclosporine or tacrolimus?
It depends on what you’re most worried about. Tacrolimus causes more tremors, sleep issues, and new-onset diabetes. Cyclosporine causes more hair growth, swollen gums, and higher cholesterol. Both damage kidneys and raise blood pressure. Tacrolimus is more potent at preventing rejection, which is why it’s used in 85% of transplants today. But if you’re struggling with neurological symptoms or diabetes, cyclosporine might be a better fit-even if it means slightly higher rejection risk.
How do I know if my tremors are from tacrolimus?
Tremors from tacrolimus are usually fine, rapid shaking in the hands, especially when holding something or trying to do fine motor tasks like writing or buttoning a shirt. They often get worse at night or when you’re stressed. If they started within weeks of beginning tacrolimus and improve when your dose is lowered, it’s likely drug-related. Your doctor can check your blood level-tremors often improve when trough levels drop from 8-10 ng/mL to 3-5 ng/mL. Never adjust your dose on your own.
Can calcineurin inhibitors cause permanent nerve damage?
In most cases, no. Neurotoxicity like tremors, headaches, and brain fog usually reverses when the dose is lowered or the drug is switched. But in rare cases, long-term exposure can lead to lasting changes. One study found subtle cognitive decline in 15-20% of long-term tacrolimus users, even after stopping the drug. That’s why some centers now do baseline and follow-up neurocognitive testing. If you notice memory problems, trouble focusing, or mood changes, talk to your doctor-don’t assume it’s just stress.
Are there natural ways to reduce side effects?
There’s no supplement or diet that can reverse the biological effects of calcineurin inhibitors. But you can support your body: eat low-sodium foods to help with blood pressure, get enough magnesium from leafy greens or supplements (as prescribed), avoid grapefruit (it interferes with drug metabolism), and stay active to improve insulin sensitivity. Never replace your meds with herbs-some, like St. John’s wort or echinacea, can trigger rejection. Always check with your transplant team before taking anything new.
How often should I get blood tests while on these drugs?
When you first start, you’ll need blood tests twice a week to check drug levels, kidney function, and electrolytes. Once stable, that usually drops to once a month. But if your dose changes, you get sick, or you start new meds, you’ll go back to weekly testing. Don’t skip them. A tiny change in your tacrolimus level can mean the difference between rejection and toxicity. Your doctor will tell you the schedule-but if you feel off, ask for a test sooner.

Janette Martens
December 28, 2025 AT 22:48#cyclosporineisabitch
Marie-Pierre Gonzalez
December 29, 2025 AT 09:29Louis Paré
December 31, 2025 AT 02:54Teresa Marzo Lostalé
December 31, 2025 AT 17:46ANA MARIE VALENZUELA
December 31, 2025 AT 20:02Bradly Draper
January 1, 2026 AT 02:13Gran Badshah
January 2, 2026 AT 08:44Samantha Hobbs
January 3, 2026 AT 21:56