What Is Autoimmune Hepatitis?
Autoimmune hepatitis (AIH) happens when your immune system mistakenly attacks your own liver. It’s not caused by alcohol, viruses, or toxins-it’s your body turning against itself. First called "lupoid hepatitis" in the 1950s, it’s now understood as a chronic condition that can quietly damage the liver for years before symptoms show up. Women are four times more likely to get it than men, and it can strike at any age, though it’s most common in your 20s or 60s. Around 10 to 25 people out of every 100,000 have it, and those numbers are rising.
The goal of treatment isn’t just to feel better-it’s to stop the liver from scarring into cirrhosis or failing entirely. Without treatment, about 50% of people with AIH will develop serious liver damage within 10 years. But with the right drugs, many can live normal, healthy lives.
How Is Autoimmune Hepatitis Diagnosed?
There’s no single test for AIH. Doctors have to piece together clues from blood work, biopsies, and ruling out other causes. If you’re feeling tired, jaundiced, or have unexplained liver enzyme spikes, your doctor will start with blood tests.
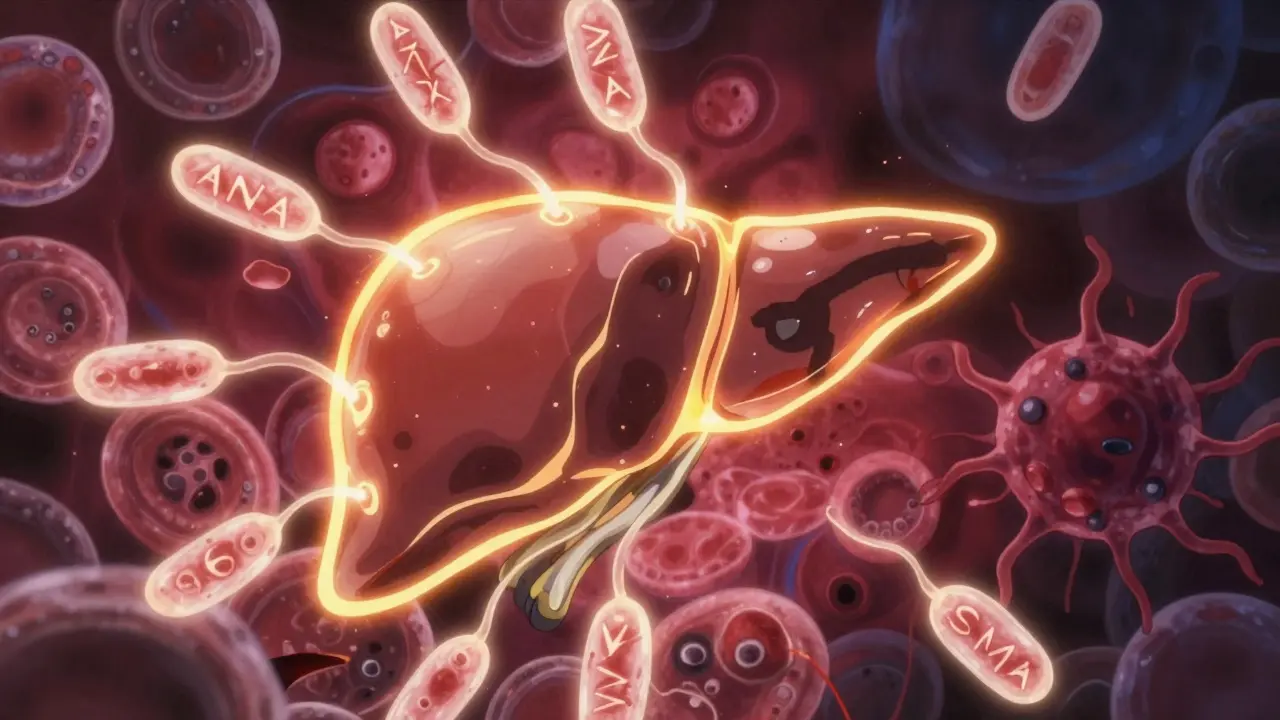
Two key markers show up in most cases: elevated immunoglobulin G (IgG)-often 1.5 times higher than normal-and specific autoantibodies. The most common are antinuclear antibodies (ANA) and smooth muscle antibodies (SMA). These are found in about 80% of cases, called Type 1 AIH. A rarer form, Type 2, shows liver-kidney microsomal antibodies (LKM1). But here’s the important part: these antibody types don’t change how you’re treated. The 2025 European guidelines stopped recommending classification by antibody type because it doesn’t affect outcomes.
The real gold standard is a liver biopsy. A small sample of liver tissue is taken with a thin needle under ultrasound guidance. The pathologist looks for "interface hepatitis"-inflammation right where the liver’s portal areas meet the tissue. This pattern is almost unique to AIH. If you see this in at least 20 portal tracts, it’s a strong sign.
Doctors also use a scoring system called the Revised IAIHG criteria. You get points for things like IgG levels, autoantibodies, liver histology, and excluding viral hepatitis. A score above 15 means probable AIH. Above 20? Definite AIH. This isn’t just academic-it helps avoid misdiagnosis. Many people are initially told they have viral hepatitis or fatty liver disease when it’s actually AIH.
Why Steroids Are the First Line of Defense
Prednisone (or its active form, prednisolone) is the cornerstone of AIH treatment. It’s a powerful corticosteroid that shuts down the immune system’s attack on the liver. Most patients start feeling better within days, and liver enzymes often drop by half in just two weeks. That rapid response is actually a diagnostic clue-if your ALT and AST levels fall fast after starting steroids, it strongly supports the AIH diagnosis.
The typical starting dose is 0.5 to 1 mg per kilogram of body weight per day, capped at 60 mg daily. That’s a lot. A 70 kg person might start at 50-70 mg. But you don’t stay there. Doctors taper it down slowly over 6 to 8 weeks to a maintenance dose of 10-15 mg daily. Why? Because long-term steroids come with serious side effects: weight gain, moon face, mood swings, high blood sugar, bone thinning, and cataracts. About 70% of people on steroids alone develop at least one of these.
But here’s the twist: steroids alone aren’t the best long-term solution. That’s where azathioprine comes in.

How Azathioprine Helps-And Why It’s Used With Steroids
Azathioprine (brand name Imuran, or generic) is an immunosuppressant that’s been used in AIH since the 1970s. It doesn’t work fast. It takes weeks to months to build up in your system. But it’s a steroid-sparer. When you combine it with prednisone, you can cut the steroid dose by 70-80% within six months. That means fewer side effects and better quality of life.
The usual starting dose is 50 mg daily, then slowly increased to 1-2 mg per kg per day, maxing out at 150 mg. It’s taken once a day, often with food to reduce stomach upset. But before you even start, your doctor should test your TPMT enzyme levels. Why? Because 0.3% of people have a genetic mutation that makes them unable to break down azathioprine. Without testing, those people risk life-threatening drops in white blood cells-up to 30 times higher risk. That test costs $250-$400, and while it’s routine in 78% of European clinics, only 45% of U.S. centers do it regularly. Don’t let this step get skipped.
Side effects of azathioprine include nausea, fatigue, and pancreatitis (which happens in about 5% of users). Bone marrow suppression-low blood counts-is the big one. That’s why blood counts are checked every 2-4 weeks at first, then monthly. If your white blood cells or platelets drop too far, the dose gets lowered or stopped.
Studies show combination therapy (steroids + azathioprine) leads to better long-term outcomes. Only 30% of people on combo therapy develop major steroid side effects, compared to 70% on steroids alone. And 60-80% of patients achieve full biochemical remission-normal liver enzymes and IgG levels-within 18 to 24 months.
What Does Remission Look Like-and Can You Stop Treatment?
Remission doesn’t mean you’re cured. It means the disease is quiet. Your ALT and AST are normal. Your IgG is back to normal. And if you’ve had a follow-up biopsy (recommended after 18-24 months), you’ll likely see the liver inflammation has cleared. In half to two-thirds of patients, the fibrosis even reverses. One patient on Reddit described going from F3 fibrosis (moderate scarring) to F0 (no scarring) after two years of treatment.
But here’s the hard truth: if you stop treatment, the disease usually comes back. Between 50% and 90% of people relapse after stopping. That’s why most people need to stay on low-dose azathioprine-sometimes for life. Some doctors try to wean patients off after 2-3 years of stable remission. They taper slowly over 6-12 months. But only about 45% of those attempts succeed. Most relapses happen within three months of stopping.
If you’re thinking about stopping, talk to your doctor. Don’t do it on your own. A relapse can mean more damage, and restarting treatment may not work as well the second time.
What If Steroids and Azathioprine Don’t Work?
Most people respond. But 10-15% don’t. That’s called treatment failure. If your liver enzymes haven’t improved after 12-18 months, your doctor will look at alternatives.
The most common second-line drug is mycophenolate mofetil (CellCept). It’s often better tolerated than azathioprine and works well for people who can’t handle the side effects. Dose is usually 1-1.5 grams twice daily. About 60-70% of non-responders improve on it.
Other options include calcineurin inhibitors like tacrolimus or cyclosporine. These are powerful and require careful monitoring of kidney function and blood levels.
Newer drugs are on the horizon. Obeticholic acid (Ocaliva), originally for primary biliary cholangitis, showed promise in a 2024 FDA breakthrough trial, with 42% of patients achieving full response versus 28% on standard therapy. JAK inhibitors like tofacitinib and monoclonal antibodies targeting IL-6 are in early trials and show over 50% response rates in small studies. These aren’t standard yet, but they’re coming.
What You Need to Do Before and During Treatment
Before starting any immunosuppressant, you must be tested for hepatitis B. About 15-20% of people carry the virus without knowing it. If you’re positive, starting steroids or azathioprine can trigger a dangerous reactivation. If you’re positive, you’ll need antiviral drugs like tenofovir before starting AIH treatment.
You should also be vaccinated for hepatitis A and B-before treatment starts. Once you’re on immunosuppressants, your body won’t respond as well to vaccines. You might only get 40-60% protection instead of the 90% you’d get when healthy.
Monitor your bones. Steroids cause osteoporosis. Ask your doctor about a DEXA scan and whether you need calcium, vitamin D, or bisphosphonates. Watch your blood sugar. Steroids can trigger diabetes. Check your weight, mood, and vision. Moon face, insomnia, and depression are common-and real.
Keep your blood tests on schedule: every 2-4 weeks early on, then every 3 months. Track your IgG levels quarterly. And if you ever feel unusually tired, have unexplained bruising, or get a fever, call your doctor. It could be a sign your blood counts are dropping.
Living With AIH: Real Stories, Real Challenges
One patient on the American Liver Foundation forum described azathioprine causing pancreatitis at 100 mg. She switched to mycophenolate and finally got stable after 18 months of trial and error. Another, on Reddit, said steroids made her unrecognizable-"moon face, 30 pounds of fluid weight in three weeks, insomnia like permanent jet lag."
But there’s hope. The same patient later said, "After two years on 5 mg prednisone and 75 mg azathioprine, my biopsy showed complete fibrosis reversal." That’s not rare. Studies confirm it happens.
65% of patients say steroid side effects are worse than the disease itself. That’s why adherence to combination therapy is higher-75% stick with it, compared to 55% on steroids alone. The key is working with your doctor to find the lowest effective dose. And remember: this isn’t a sprint. It’s a marathon. The goal isn’t just to survive-it’s to thrive.
What’s Next for AIH Treatment?
The 2025 EASL guidelines are the most important update in a decade. They’ve simplified diagnosis, extended the window for assessing treatment response to 6-12 months, and removed outdated antibody-based subtyping. More centers are now doing TPMT testing, and more patients are getting biopsies to confirm remission.
Research is moving fast. Scientists are looking at genetic markers like HLA-DRB1*03:01 and *04:01 to predict who’ll have severe disease. Blood tests for microRNA patterns are showing 85% accuracy in predicting steroid response within two weeks. That could mean personalized treatment plans-no more guessing.
For now, steroids and azathioprine remain the standard. But the future is brighter. Better drugs are coming. Better monitoring is here. And more patients are surviving-not just living-with AIH.
Solomon Ahonsi
February 3, 2026 AT 01:10George Firican
February 5, 2026 AT 00:27Matt W
February 6, 2026 AT 15:39Anthony Massirman
February 7, 2026 AT 04:31Monica Slypig
February 7, 2026 AT 14:40Becky M.
February 8, 2026 AT 08:49Dan Pearson
February 9, 2026 AT 09:27Eli Kiseop
February 10, 2026 AT 17:51Ellie Norris
February 11, 2026 AT 22:45Marc Durocher
February 13, 2026 AT 18:37larry keenan
February 14, 2026 AT 09:29Nick Flake
February 15, 2026 AT 19:26Akhona Myeki
February 17, 2026 AT 05:58Chinmoy Kumar
February 19, 2026 AT 02:24Brett MacDonald
February 19, 2026 AT 03:59