Imagine sitting in a classroom while the teacher speaks, but the words come in like broken radio signals-some clear, others lost in static. You hear the sounds, but the meaning slips away. This isn’t daydreaming. It’s not laziness. For children and adults with auditory processing disorder (APD), listening is a constant, exhausting battle-even when their ears work perfectly.
What Is Auditory Processing Disorder?
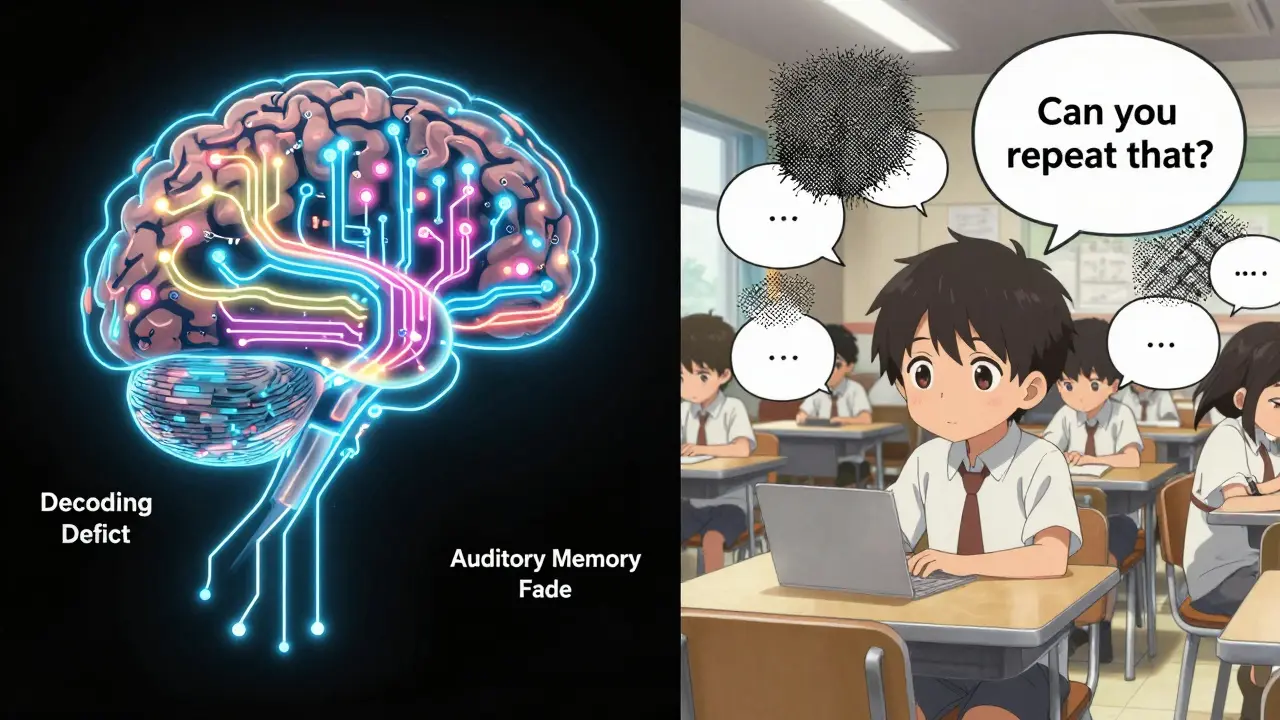
Auditory Processing Disorder, also called Central Auditory Processing Disorder (CAPD), isn’t hearing loss. People with APD can hear quiet sounds just fine on a standard hearing test. The problem isn’t in the ears-it’s in the brain. The auditory nerve sends the sound signal to the brain, but the brain struggles to organize, interpret, or make sense of it. It’s like having a high-speed internet connection but a slow, glitchy router that can’t decode the data properly. This condition affects about 3% to 5% of school-aged children, and it shows up more often in boys than girls. Adults can have it too, often undiagnosed until they hit environments with complex listening demands-like meetings with background chatter or group conversations. Unlike hearing loss, which shows up on a pure-tone audiogram as elevated thresholds, APD shows up only on specialized tests that measure how the brain processes sound.How APD Affects Listening
The brain doesn’t process all sounds the same way. APD breaks down in specific areas:- Auditory discrimination: Telling the difference between similar sounds like “bat” and “pat.”
- Listening in noise: Understanding speech when there’s background noise-like a cafeteria or a busy street. This is the #1 challenge, affecting 78% of diagnosed kids.
- Auditory memory: Forgetting spoken instructions after just a few seconds. “Go get your shoes, then brush your teeth, then come downstairs” becomes a blur.
- Sound localization: Not knowing where a sound is coming from. You turn around when someone calls your name… but they’re right beside you.
- Timing and rhythm: Missing subtle pauses or overlaps in speech, making fast talkers or overlapping conversations impossible to follow.
Why APD Gets Misdiagnosed
APD looks a lot like ADHD. Both involve trouble focusing in noisy rooms. Both lead to forgetfulness and poor following of directions. In fact, 30% to 40% of kids with APD also have ADHD. But the root cause is different. With ADHD, the brain struggles to filter out distractions. With APD, the brain can’t even decode the signal properly. One child might zone out because they’re bored. Another might zone out because they literally can’t make out what’s being said. The fix isn’t the same. It also overlaps with dyslexia. About 25% to 35% of children with APD also have trouble with reading. That’s because reading depends on being able to hear and manipulate sounds within words. If your brain can’t tell the difference between “d” and “t,” learning phonics becomes a nightmare. Many kids get sent for speech therapy or behavioral interventions before anyone checks their auditory processing. A 2021 study found that 45% of children referred for APD testing actually had attention or language issues instead. That’s why diagnosis isn’t just one test-it’s a full battery.How APD Is Diagnosed
A regular hearing test won’t catch APD. You need a certified audiologist who specializes in central auditory processing. The process usually takes two to three sessions and includes:- Dichotic Digits Test: Different numbers are played into each ear at the same time. The person must repeat them back. People with APD often mix them up.
- Random Gap Detection Test: Measures how well the brain detects tiny pauses between sounds. A delay of just 20 milliseconds can be missed.
- Pitch Pattern Sequence Test: Listens to rising and falling tones and must repeat the pattern. This checks timing and sequencing skills.
Types of APD
Not all APD is the same. Experts like Dr. Teri James Bellis describe four main subtypes:- Decoding deficit: Trouble distinguishing sounds. Often linked to left-brain issues. This is the most common type and overlaps with reading problems.
- Tolerance-fading memory deficit: Can’t hold onto what’s heard, especially if the sound is fuzzy or quiet. Memory fades fast.
- Auditory integration deficit: Can’t combine information from both ears. Like trying to listen with one ear plugged.
- Prosodic deficit: Misses tone, emotion, or sarcasm in speech. Sounds flat. May seem emotionally disconnected.
What Doesn’t Work
There’s no pill for APD. Medications used for ADHD won’t fix it. You can’t “train” someone to hear better with simple ear exercises. And no, turning up the volume won’t help if the brain can’t process the signal. Some programs promise quick fixes-apps that claim to “rewire” the brain in weeks. These often lack scientific backing. The American Speech-Language-Hearing Association warns against overdiagnosis and unproven treatments. Real progress comes from structured, evidence-based approaches.What Actually Helps
The good news? APD can be managed. With the right support, kids thrive. Environmental changes: Simple adjustments make a huge difference. Preferential seating-within 3 to 6 feet of the teacher-reduces distance and noise. Sound-field amplification systems in classrooms boost the teacher’s voice above background noise by 15 to 20 decibels. That’s like turning up the speaker, but without making it loud for everyone else. Assistive tech: FM systems (a mic worn by the teacher, a receiver in the child’s ear) are highly effective. Personal sound amplification products (PSAPs) are becoming more affordable and targeted. Speech-language therapy: Focused on metacognitive strategies-teaching kids to ask for repetition, summarize what they heard, and use context clues. One 2022 ASHA review found these approaches improved academic outcomes in 70% of cases. At-home strategies: Reduce background noise during homework. Use visual cues-written instructions, charts, pictures. Break down multi-step tasks. Practice active listening: “Can you tell me what you heard?” Auditory training: Programs like Earobics, used in controlled studies, show 40% to 60% improvement in sound discrimination after 10 to 12 weeks of daily 15-minute sessions.
Support in School and Work
In the U.S., children with APD qualify for accommodations under IDEA or Section 504. That means:- Extra time on verbal tests
- Written copies of instructions
- Use of note-takers or audio recordings
- Preferential seating
- Avoidance of rapid-fire questioning
Long-Term Outlook
APD doesn’t go away, but it doesn’t have to hold you back. A 10-year study from the University of Florida found that 80% of children who received early, consistent support developed strong compensatory strategies and succeeded academically. But 45% of adults still struggle in noisy environments. That’s why self-advocacy matters. Teaching kids to say, “I didn’t catch that-can you repeat it?” or “Can you write that down?” is as important as any therapy. The brain is adaptable. With the right tools, people with APD learn to navigate a world built for neurotypical listeners. They become experts at reading lips, using context, and asking for help. Many go on to become teachers, writers, engineers-people who’ve learned to turn their challenge into strength.What You Can Do
If you suspect APD in yourself or your child:- Track the patterns. Does the person mishear instructions often? Do they say “huh?” or “what?” in quiet rooms too?
- Rule out hearing loss with a standard audiogram.
- Find a pediatric or adult audiologist trained in APD testing. Ask if they use the Dichotic Digits, Random Gap, and Pitch Pattern tests.
- Request an evaluation through your school district or workplace if applicable.
- Start low-cost, high-impact changes: reduce background noise, use visuals, speak clearly and slowly.
- Connect with communities like Reddit’s r/APD. You’re not alone.
Is auditory processing disorder the same as hearing loss?
No. Hearing loss means the ears can’t pick up sounds clearly-there’s physical damage or blockage. APD means the ears work fine, but the brain struggles to interpret what the ears hear. A standard hearing test will come back normal for someone with APD, but specialized tests will show processing gaps.
Can adults be diagnosed with APD?
Yes. While APD is often noticed in childhood when school demands increase, many adults go undiagnosed until they face noisy workplaces, group meetings, or fast-paced conversations. Symptoms like constant mishearing, fatigue after listening, or avoiding social situations can be signs. Audiologists can test adults using the same protocols as children.
Does APD mean someone is lazy or not paying attention?
Absolutely not. People with APD aren’t ignoring you-they’re working harder than most to understand what’s being said. What looks like inattention is actually auditory overload. They’re not choosing to miss information; their brain is literally processing it differently. Calling them lazy makes the struggle worse.
Are there medications for APD?
No. There are no drugs approved or proven to treat APD. Medications for ADHD or anxiety won’t fix the underlying auditory processing issue. Treatment focuses on environmental changes, assistive technology, speech therapy, and auditory training-not pills.
Can APD be cured?
There’s no cure, but there is significant improvement. With early intervention and consistent support, most children develop coping strategies that allow them to succeed in school and work. The brain can adapt. While the processing difference remains, people learn to work around it-just like someone with dyslexia learns to read differently.
How common is APD in adults?
Exact numbers aren’t known, but research suggests it’s underdiagnosed. About 82% of adults with APD report workplace listening challenges, especially in meetings or noisy offices. Many assume they’re just “bad listeners,” not realizing it’s a neurological difference. As awareness grows, more adults are getting tested and finding relief through accommodations.

Kathy Scaman
January 28, 2026 AT 11:59My brother had this and no one figured it out until he was 16. Thought he was just zoning out. Turns out he was trying to decode sentences like they were Morse code. Teachers called him lazy. He just couldn’t keep up with the noise.
Now he’s a software dev. Uses noise-canceling headphones and writes everything down. No meds. Just adaptations.
Phil Davis
January 28, 2026 AT 19:56So let me get this straight-your brain’s like a WiFi router that got stuck on 2.4GHz while everyone else is on 5G?
Kinda makes you wonder how we ever built civilization with so many people running on faulty firmware.
Mindee Coulter
January 28, 2026 AT 22:34I work in a call center and I’ve been saying for years I can’t follow conversations in the break room. Finally got tested last year. APD. No one believed me until the audiologist showed me the data.
Now I ask for emails after every meeting. No shame.
Bryan Fracchia
January 29, 2026 AT 13:08It’s wild how much we assume listening is passive. Like if you’ve got ears, you’re good to go.
But your brain’s the real decoder. And if that’s glitchy, no amount of ‘pay attention’ fixes it.
People with APD aren’t broken-they’re just running a different OS. We need more compatibility patches, not blame.
Timothy Davis
January 31, 2026 AT 03:06Let’s be real-this is just ADHD with a fancy label. 3% of kids? More like 3% of parents who don’t want to discipline their kids.
My kid gets distracted? We turn off the TV. Done.
Stop pathologizing normal behavior.
Sue Latham
January 31, 2026 AT 10:13Oh honey, if you’re struggling to hear in a cafeteria, maybe you just need to stop hanging out with the riffraff.
Real intellectuals don’t speak over each other. And if you can’t keep up with basic conversation, maybe you’re not meant for the real world.
Also, FM systems? That’s just coddling. Build resilience.
Amber Daugs
February 1, 2026 AT 19:42I’m a teacher. I’ve seen this ‘APD’ nonsense for years. It’s just a way for parents to avoid responsibility.
My kid has to sit still and listen. Why can’t yours?
And don’t get me started on those ‘sound-field amplification systems’-we’re not running a radio station here.
James Dwyer
February 2, 2026 AT 00:50My daughter was diagnosed at 8. We started using visual schedules and written notes. Within months, she went from crying over homework to acing her spelling tests.
It’s not magic. It’s just meeting people where they are.
And yeah-it’s hard to fight the system. But it’s worth it.
jonathan soba
February 2, 2026 AT 21:05Interesting how the American medical-industrial complex keeps inventing new disorders so they can sell you more devices.
Meanwhile, in Europe, we just teach kids to adapt. No tech. No accommodations. Just discipline.
Maybe we should stop treating incompetence like a disability.
matthew martin
February 3, 2026 AT 12:32APD is like trying to read a book where every other word is scribbled out with a crayon.
You can see the letters. You know the language. But your brain’s stuck in a loop trying to guess what’s missing.
That’s why ‘just focus’ doesn’t work. It’s not focus-it’s perception.
And honestly? The fact that we’re even having this conversation means we’re finally starting to see people, not just behaviors.
Chris Urdilas
February 4, 2026 AT 16:13So you’re telling me the entire education system is built for neurotypical brains and we’re surprised when some kids fall through?
Of course they do.
Let’s not act like this is new. We’ve been ignoring this for decades.
Now we’re just slapping a label on it and calling it progress.
Meanwhile, the real win is the kid who finally gets a quiet corner and a written list.
That’s not therapy. That’s basic human decency.
Irebami Soyinka
February 6, 2026 AT 10:31Why do Americans always need a medical diagnosis for everything?
In Nigeria, we just say ‘he’s slow to understand’ and push harder.
They don’t get special chairs or microphones. They get told to listen better.
And guess what? They still grow up. Stronger.
Maybe stop coddling and start challenging.
SRI GUNTORO
February 7, 2026 AT 19:34My cousin had this. She was labeled lazy. Her parents didn’t believe in ‘brain disorders.’ She dropped out at 15.
Now she works as a cleaner. She says she can’t handle crowds.
It’s tragic. And it’s because people like you don’t take it seriously.
Stop pretending it’s not real.
Anna Lou Chen
February 8, 2026 AT 00:45Deconstructing the auditory hegemony: APD as a symptom of late-capitalist cognitive overstimulation, wherein the neurodivergent subject is pathologized for failing to optimize their perceptual throughput within a hyper-linguistic, neoliberal regime of attentional extraction.
But let’s not forget-the body is not a machine. The ear is not a transducer. The brain is not a processor.
It’s all semiotics, baby.
And the real solution? Deconstruct the classroom. Abolish the lecture. Let silence breathe.