Herbal Supplement & Blood Thinner Interaction Checker
Select Your Blood Thinner
Select Your Supplements
When you’re on a blood thinner like warfarin, apixaban, or rivaroxaban, your body is walking a tightrope. Too much thinning, and you risk a dangerous bleed. Too little, and a clot could form-potentially causing a stroke or heart attack. Now add herbal supplements into the mix, and that tightrope gets even narrower. Many people assume that because something is "natural," it’s safe. But when it comes to blood thinners, that belief can land you in the emergency room.
Why Herbal Supplements Can Be Dangerous with Blood Thinners
Herbal supplements don’t come with warning labels like prescription drugs. You won’t find a sticker on a bottle of ginkgo or garlic saying, "May cause severe bleeding when taken with warfarin." Yet that’s exactly what can happen. These supplements interfere with how your body processes anticoagulants-either by changing how much of the drug gets into your bloodstream or by directly boosting its blood-thinning effect. Take warfarin, for example. It’s broken down in the liver by enzymes called CYP2C9 and CYP3A4. Certain herbs block these enzymes, causing warfarin to build up in your blood. Danshen (Salvia miltiorrhiza), a herb commonly used in traditional Chinese medicine, can spike your INR-a measure of how long it takes your blood to clot-by 300% to 400% within just three days. That’s not a minor fluctuation. That’s a medical emergency waiting to happen. Other herbs don’t change drug levels at all. Instead, they work directly on your blood’s clotting system. Ginkgo biloba, for instance, inhibits platelet-activating factor, making platelets less likely to stick together. When you combine that with warfarin, you’re essentially double-dosing your blood’s ability to thin. Garlic, ginger, and ginseng do similar things. Even green tea, often seen as harmless, contains compounds that can interfere with clotting factors.The Top 10 Herbal Risks You Can’t Ignore
Based on over 14,000 adverse event reports analyzed by the FDA in 2024, these 10 supplements are the most dangerous when taken with anticoagulants:- Ginkgo biloba
- Garlic
- Ginger
- Ginseng
- St. John’s Wort
- Chamomile
- Cranberry
- Green tea
- Chinese wolfberry (goji berry)
- Dong quai
St. John’s Wort: The Silent Killer
Not all interactions make your blood thinner. Some make it thicker-just as dangerous. St. John’s Wort, often used for mild depression, is a powerful inducer of liver enzymes. It speeds up the breakdown of anticoagulants like apixaban and rivaroxaban, dropping their blood levels by up to 50% within 72 hours. That means your medication stops working. You’re no longer protected from clots. A 2021 study in Clinical Pharmacology & Therapeutics showed that patients taking apixaban and St. John’s Wort had clotting events within days of starting the herb. One patient developed a pulmonary embolism after combining the two. He had no idea the supplement could undo his medication. This isn’t just about warfarin. Newer anticoagulants like apixaban, dabigatran, and edoxaban were designed to be safer and more predictable. But they’re not immune. St. John’s Wort remains one of the most under-recognized threats in modern anticoagulant therapy.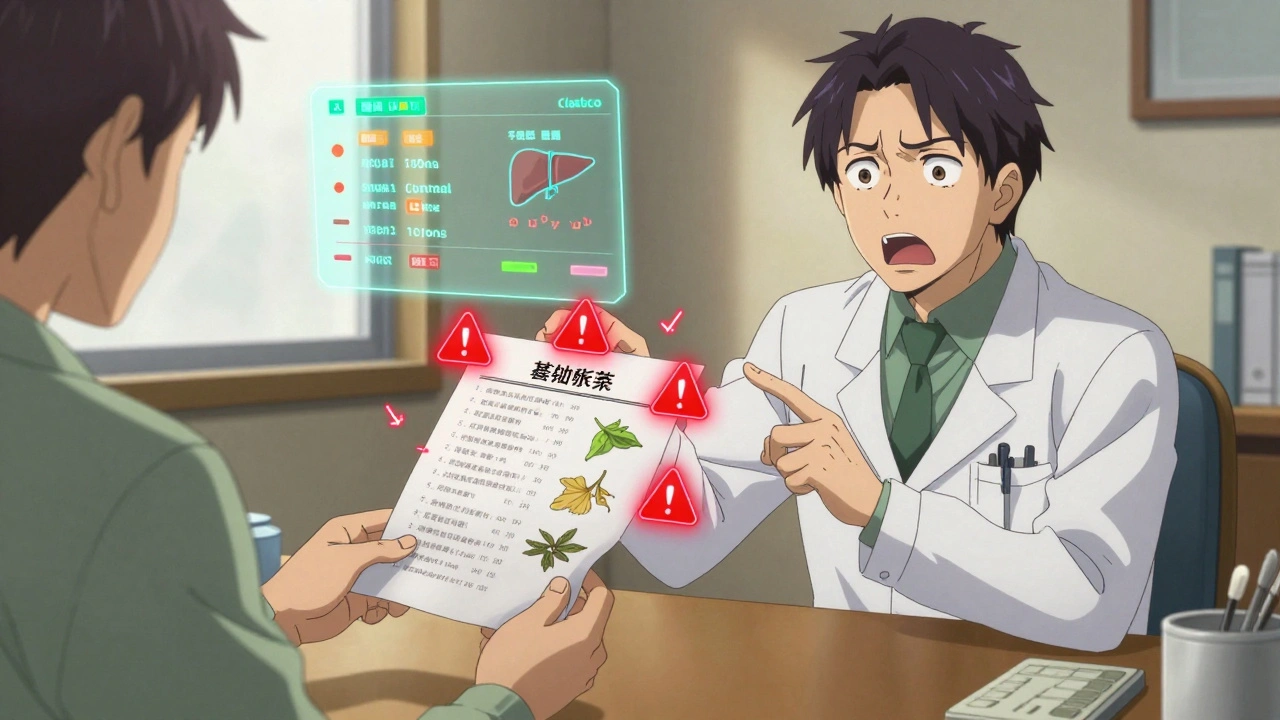
Why Doctors Often Miss This
If you’re on a blood thinner, your doctor checks your INR, asks about other medications, and probably talks to you about diet. But how often do they ask: "Are you taking any herbal supplements?" The data says: not often enough. A 2022 study found that while 89% of doctors asked about prescription drugs, only 37% specifically asked about herbs. And even when patients mentioned them, only 27% of those conversations were documented in medical records. Part of the problem is time. A typical visit lasts 15 minutes. But the bigger issue is assumption. Many providers still think herbal supplements are harmless or that patients wouldn’t use them. That’s outdated thinking. Nearly half of Americans over 65 take herbal supplements while also on anticoagulants, according to the NCCIH 2024 survey. Some clinics are changing this. The University of California San Francisco Medical Center introduced a simple 5-step screening tool in 2023. Within 18 months, undocumented supplement use dropped from 73% to 28%. All it took was asking the right question: "What vitamins, herbs, or supplements do you take daily?"What About CBD Oil? The New Wild Card
CBD oil has exploded in popularity. People use it for sleep, anxiety, pain. But it’s not the harmless wellness trend it’s made out to be when paired with blood thinners. A 2024 randomized trial in JAMA Internal Medicine found that CBD oil increased INR levels by 2.8 times in 68% of warfarin users. That’s not a small bump. That’s a red flag. CBD inhibits the same liver enzymes as danshen and ginkgo, leading to dangerous drug buildup. And because CBD products aren’t regulated, you don’t even know how much you’re getting. One bottle might have 10mg per serving. Another might have 50mg. No way to predict the effect. The FDA hasn’t issued formal warnings yet, but clinicians are already seeing cases. One patient in Ohio had a brain bleed after starting CBD for back pain. His INR was 8.6-more than double the safe range.What You Can Do Right Now
If you’re on a blood thinner, here’s what you need to do:- Make a list. Write down every supplement, herb, vitamin, or tea you take daily-even if you think it’s harmless.
- Bring it to every appointment. Don’t wait for your doctor to ask. Show them the list. Say: "I’m on a blood thinner. Are any of these unsafe?"
- Check with your pharmacist. Pharmacists are trained in drug interactions. They can check the Natural Medicines Database, which rates interactions on a scale from 1 (minor) to 7 (life-threatening). Anything rated 5 or higher? Stop it.
- Don’t start anything new without checking. Even "mild" herbs like turmeric or ginger can be risky. A Reddit user named u/WarfarinWarrior spiked his INR to 4.2 after adding turmeric to his morning smoothie. He ended up in the hospital.
- Know your INR. If your INR is stable, don’t let a new supplement throw it off. A change of 0.5 or more in INR can mean the difference between safety and bleeding.


Constantine Vigderman
December 13, 2025 AT 10:10Cole Newman
December 14, 2025 AT 18:01Casey Mellish
December 16, 2025 AT 07:07Tyrone Marshall
December 16, 2025 AT 14:03Emily Haworth
December 17, 2025 AT 20:39Tom Zerkoff
December 18, 2025 AT 06:46Yatendra S
December 18, 2025 AT 15:14Himmat Singh
December 19, 2025 AT 19:00kevin moranga
December 21, 2025 AT 11:00