Amlodipine Eye Health Tracker
Track Your Eye Symptoms
Use this tool to assess your risk of vision-related side effects from amlodipine. Based on your inputs, we'll provide personalized recommendations.
Quick Takeaways
- Amlodipine can cause blurry vision, dry eye, and in rare cases retinal issues.
- Most eye side effects appear within the first few weeks of treatment.
- Regular eye checks and reporting symptoms early can prevent permanent damage.
- Switching to another calcium channel blocker or adjusting dose often resolves problems.
- Never stop the medication without a doctor's guidance.
When you pick up a prescription for Amlodipine is a calcium channel blocker used to treat hypertension and angina, the focus is usually on blood pressure control. But a side effect that often flies under the radar is how the drug can affect your eyesight. If you’ve noticed new floaters, a dry sensation, or sudden blurriness, you’re not alone-many patients report subtle changes in vision after starting the medication.
How Amlodipine Works (and Why Eyes Can Feel the Impact)
Amlodipine belongs to the Calcium channel blocker family, which relaxes the smooth muscles in blood vessel walls. By blocking calcium influx, the arteries widen, lowering the workload on the heart. The same vasodilatory effect reaches the tiny vessels that feed the retina and the optic nerve. When those vessels adjust too quickly, fluid balance can shift, leading to visual disturbances.
Most patients tolerate the medication well, but the eye’s delicate micro‑circulation can react differently than larger vessels. Understanding the mechanism helps explain why some people notice changes within days while others never see a difference.
Common Ocular Side Effects Reported with Amlodipine
Clinical trials and post‑marketing reports list several eye‑related complaints. Here’s what shows up most often:
- Blurred vision - a hazy or out‑of‑focus feeling that can come on gradually.
- Dry eye sensation - a gritty feeling, often worse in dry climates or after long screen time.
- Increased light sensitivity - eyes may feel uncomfortable in bright environments.
- Rarely, retinal pigment epithelium changes or even detachment - these are serious but extremely uncommon.
Most of these symptoms are classified as Vision changes and are reversible once the underlying cause is addressed.
Frequency, Risk Factors, and Who’s Most Affected
Studies show that about 5‑10% of patients on amlodipine report some form of visual disturbance, with blurred vision being the most frequent. Risk spikes for people who:
- Already have eye conditions such as glaucoma or macular degeneration.
- Take multiple antihypertensive drugs that also affect blood flow.
- Are older than 65 - the retinal vessels become less elastic with age.
- Live in high‑altitude or low‑humidity environments, which can exacerbate dry eye.
If you fall into any of these groups, keep a closer eye (pun intended) on any visual shifts during the first month of therapy.
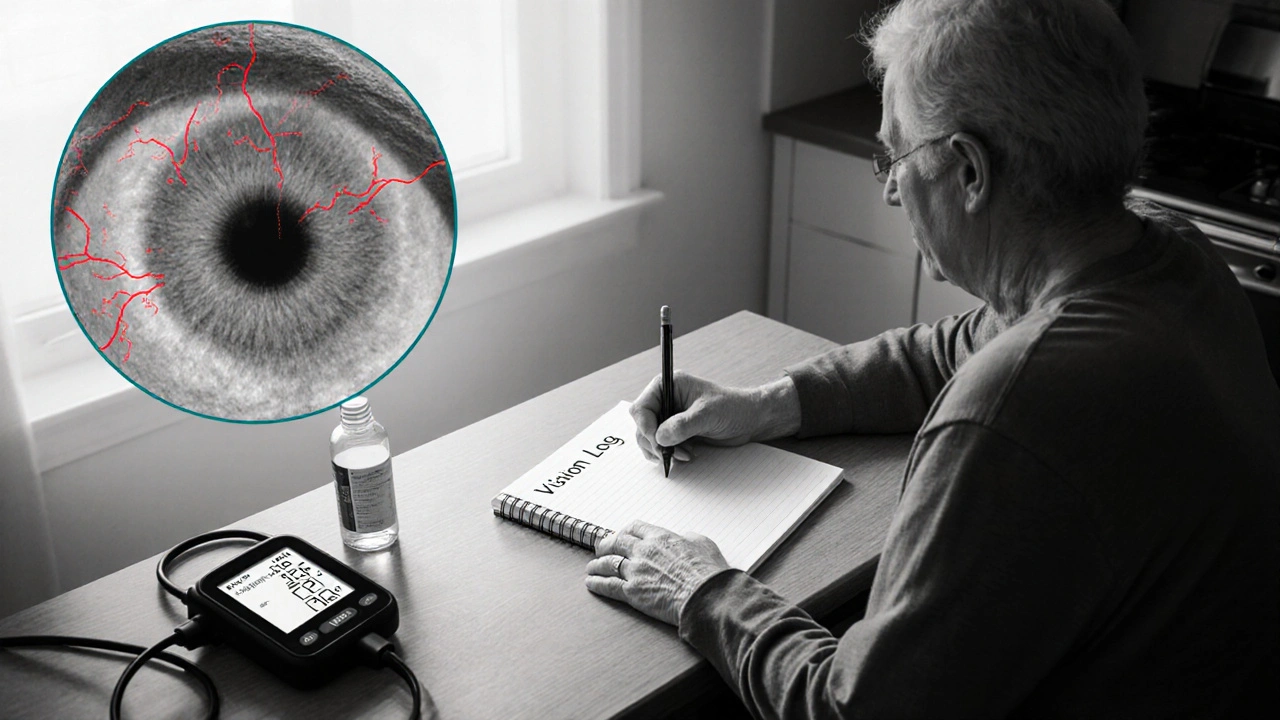
How to Monitor Your Vision While on Amlodipine
Self‑tracking is simple and can catch problems early:
- Baseline check: Before starting the drug, note any existing vision issues. A quick appointment with an Ophthalmologist can establish a reference point.
- Weekly log: Write down any new floaters, blurriness, or eye discomfort. Include the time of day and activities (e.g., reading, driving).
- Eye‑drop trial: If dryness appears, over‑the‑counter lubricating drops can relieve symptoms while you assess whether the problem persists.
- Blood pressure correlation: Note if vision changes coincide with spikes or drops in your Hypertension readings. Fluctuations might hint that the medication dose needs tweaking.
When symptoms linger beyond two weeks or worsen suddenly, it’s time to act.
When to See an Eye Specialist
Schedule an appointment if you experience any of the following:
- Sudden loss of peripheral vision or a curtain‑like shadow.
- Persistent double vision.
- Eye pain that doesn’t improve with rest.
- Unexplained flashes of light or a surge of new floaters.
These signs could point to retinal detachment or vascular events, which need prompt treatment. Even milder complaints deserve a check‑up if they interfere with daily tasks like reading or driving.
Managing Side Effects Without Stopping the Medication
Doctors rarely ask patients to quit amlodipine abruptly because uncontrolled blood pressure carries greater risks than most eye complaints. Here are some strategies that keep both heart and eyes happy:
- Dose adjustment: Lowering the dose by 2.5mg can reduce ocular symptoms while still controlling blood pressure.
- Switch to another calcium channel blocker: Nifedipine or diltiazem have slightly different vessel‑targeting profiles and may cause fewer eye issues.
- Adjunct therapies: Adding a short‑acting diuretic can smooth out blood‑pressure swings that trigger vision changes.
- Supportive eye care: Regular use of preservative‑free artificial tears, humidifiers at work, and protective sunglasses can mitigate dryness and light sensitivity.
Any change should be made under a physician’s guidance, but most patients find relief within a few weeks.
Comparison of Ocular Side Effects Among Common Calcium Channel Blockers
| Drug | Blurred Vision | Dry Eye | Retinal Issues (rare) | Typical Dose Range (mg) |
|---|---|---|---|---|
| Amlodipine | 5‑10% | 3‑7% | 0.1% | 2.5‑10 |
| Nifedipine | 3‑8% | 2‑5% | 0.05% | 10‑60 |
| Verapamil | 2‑6% | 1‑4% | 0.02% | 80‑240 |
| Diltiazem | 4‑9% | 3‑6% | 0.07% | 30‑360 |
Numbers reflect pooled data from clinical trials and post‑marketing surveillance. Amlodipine’s rates sit in the middle of the pack-neither the safest nor the most problematic.
Key Takeaway: Keep an Eye on Your Eyes
While amlodipine does a solid job of keeping Blood pressure in check, it can also nudge the eye’s micro‑circulation. The good news is that most side effects are mild, reversible, and manageable with a few practical steps. By staying aware of any visual shifts, logging them, and talking to your doctor or ophthalmologist early, you can protect both your heart and your sight.
Frequently Asked Questions
Can amlodipine cause permanent vision loss?
Permanent loss is extremely rare. Most reported issues, like blur or dryness, improve after dose adjustment or a switch to another medication.
How long after starting amlodipine might I notice eye changes?
Symptoms usually appear within the first two to four weeks, but some patients report changes as early as a few days.
Should I stop the drug if I get blurry vision?
Never stop without consulting your prescriber. Sudden discontinuation can spike blood pressure and increase cardiovascular risk.
Are there any eye‑friendly alternatives to amlodipine?
Other calcium channel blockers like nifedipine or diltiazem have slightly different side‑effect profiles. ACE inhibitors or ARBs are also effective for hypertension and generally have fewer ocular complaints.
What tests will an ophthalmologist run if I report symptoms?
A standard eye exam includes visual acuity, dilated fundus photography, and optical coherence tomography (OCT) to check the retina and optic nerve for any subtle changes.

Roberta Makaravage
October 17, 2025 AT 02:18Life isn’t just about keeping blood pressure low; it’s also about safeguarding the windows to our soul. When a medication like amlodipine starts to blur those windows, we have an ethical duty to notice and act. Ignoring a dry eye isn’t just discomfort; it’s a subtle erosion of quality of life that we, as responsible patients, must confront. The micro‑circulation of the retina is a delicate tapestry, and tampering with it without vigilance borders on negligence. Each blink of irritation is a tiny alarm bell, urging us to log the symptom and reach out to a specialist. It’s not enough to trust that “everyone else gets through it fine”; individual variance demands personal attention. Moreover, the pharmaceutical industry may downplay ocular side‑effects to keep sales soaring, so we must be our own advocates. Remember, the principle of “first, do no harm” extends beyond the heart to the eyes. 🌟 If you spot a new floaters or a sudden glare, write it down, note the time, and compare it to your blood pressure trends. This practice creates a data trail that can sway a doctor toward dose adjustment before irreversible damage sets in. Treat your vision log like a moral ledger-each entry is a testament to self‑respect. While the drug saves your heart, you must safeguard your sight with equal fervor. Reflexive vigilance is a form of gratitude toward both your body and the science that crafted the pill. The moment you dismiss a mild blur as “just aging” you surrender a piece of your autonomy. 🙁 So, commit to weekly checks, use preservative‑free tears if needed, and never shy away from asking the hard questions. In the grand tapestry of health, your eyes deserve a starring role, not a footnote. 🌈
Lauren Sproule
October 30, 2025 AT 22:38Hey folks just wanted to chime in that i think staying on top of any eye changes is super important i mean it’s not rocket science just keep a little notebook and jot things down if you feel dry or blurry definitely talk to ur doc they’ll help figure it out 🙌
CHIRAG AGARWAL
November 13, 2025 AT 19:58Honestly this whole amlodipine eye thing sounds overhyped. If you’re getting a little blur, maybe it’s just your brain not the pill.
Rebecca Mitchell
November 27, 2025 AT 17:18Eye dryness? Try drops.
Katie Henry
December 11, 2025 AT 14:38Dear readers, it is imperative to monitor ocular symptoms diligently while on amlodipine. Regular ophthalmic evaluations represent a prudent safeguard against potential complications. I encourage you to maintain a systematic log of any visual disturbances. By doing so, you empower your healthcare provider to make informed adjustments, thereby preserving both cardiovascular and visual health.
Joanna Mensch
December 25, 2025 AT 11:58Some folks don’t realize that pharmaceutical companies often suppress data about rare side‑effects to protect profits. It wouldn’t surprise me if there are undisclosed studies linking amlodipine to more serious retinal issues. Stay skeptical and demand full transparency.
RJ Samuel
January 8, 2026 AT 09:18Well, I’ll be the first to say that the hype around amlodipine’s eye risks is a bit of a dragon’s tail-fluffy and overblown. While a sprinkle of dryness can happen, the vast majority sail through without a hitch. If you’re itching for drama, look at the comparative stats: nifedipine and diltiazem have their own quirks, so the blame game is futile. In short, keep your eyes peeled, but don’t let every sneeze become a prophecy of blindness. Embrace the nuance, not the alarmist chorus.
Chris Beck
January 22, 2026 AT 06:38Look, the drug works good!! but some people whine about eye stuff... it's not a death sentence. Just get checked and move on!!
James Falcone
February 5, 2026 AT 03:58Enough with the fear mongering. If you have a problem, see a doc, otherwise keep taking it.