Most people think a bad cough means they need antibiotics. But if you’ve been coughing for more than a few days with no fever, no trouble breathing, and no chest pain, you probably have acute bronchitis - and antibiotics won’t help. In fact, they might make things worse.
What Exactly Is Acute Bronchitis?
Acute bronchitis is an inflammation of the bronchial tubes - the airways that carry air to your lungs. It’s not pneumonia. It’s not a cold. It’s a viral infection that starts in your upper respiratory tract and moves down, irritating the lining of your airways. The result? A cough that can last for weeks. It’s one of the most common reasons people visit their doctor. In the U.S., about 10 million visits each year are for acute bronchitis. Most of the time, it’s caused by viruses - rhinovirus (the common cold), flu, coronavirus, or RSV. Bacteria? Rare. Less than 10% of cases. The cough is the main symptom. It might start dry, then turn wet with clear or white mucus. You might feel tired, have a mild sore throat, or feel a bit achy. But if you have a fever over 38°C, rapid breathing, or chest pain that gets worse when you breathe, that’s not bronchitis - that’s pneumonia. See a doctor right away.How Long Does the Cough Last?
This is where most people get frustrated. You expect to feel better in a few days. But with acute bronchitis, the cough lingers. Studies show:- 50% of people are still coughing at 10 days
- 26% are coughing at 14 days
- 11% are coughing at 21 days
Why Antibiotics Don’t Work (and Why They’re Dangerous)
Antibiotics kill bacteria. They don’t touch viruses. And since 90-95% of acute bronchitis cases are viral, antibiotics are useless here. But here’s the scary part: even though doctors know this, they still prescribe antibiotics in more than half of cases. In some parts of the U.S., the rate hits 78%. Why? Because patients ask for them. Because doctors feel pressured. Because it’s easier than explaining why you don’t need them. The truth? Antibiotics give you almost no benefit. A major review of nine studies with over 5,600 patients found antibiotics reduce cough duration by just 0.6 days. That’s less than half a day. Meanwhile, 1 in 14 people gets side effects - nausea, diarrhea, rash, or yeast infections. And that’s just the personal cost. The bigger problem is antibiotic resistance. Every unnecessary antibiotic you take helps superbugs grow. The CDC says respiratory infections like bronchitis drive 46 million unnecessary antibiotic prescriptions in the U.S. each year. That’s part of why 2.8 million people get antibiotic-resistant infections annually - and 35,000 die.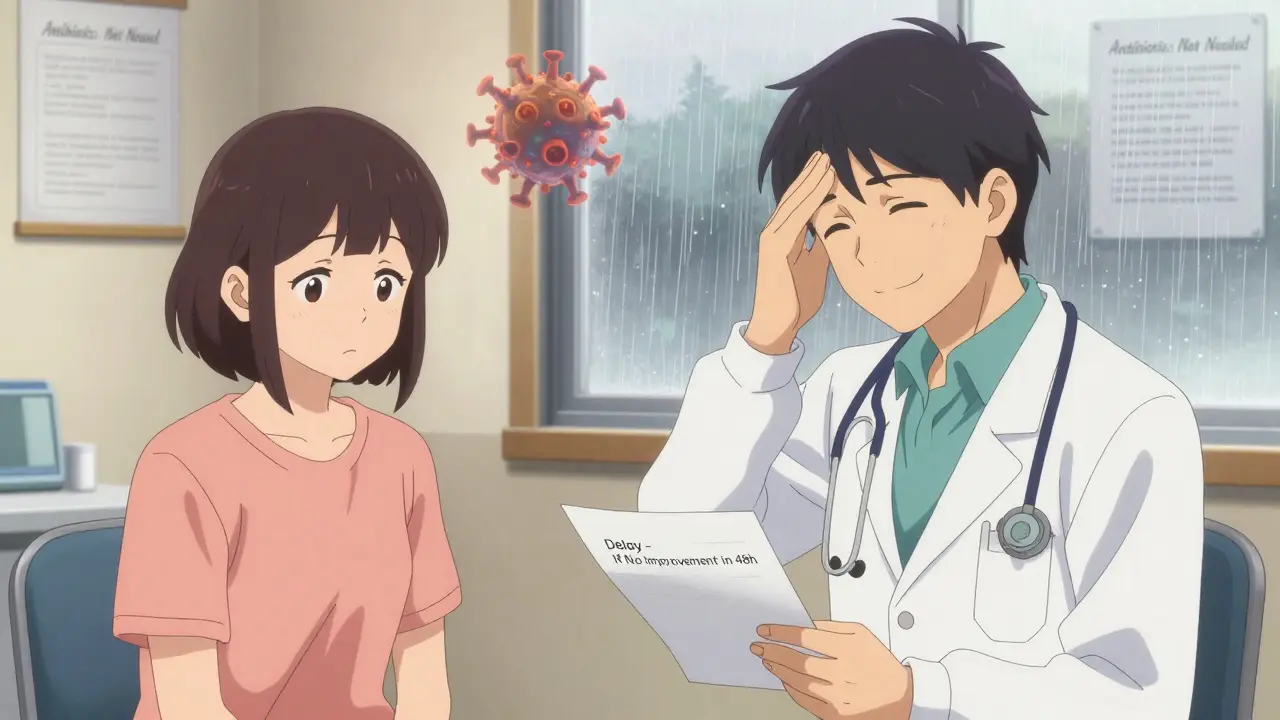
What Actually Helps? Evidence-Based Cough Care
You don’t need antibiotics. But you do need relief. Here’s what works - backed by science:1. Honey
Honey is one of the best cough remedies you already have in your kitchen. A 2018 study in JAMA Pediatrics found honey worked as well as over-the-counter cough medicine in kids - and better than nothing. For adults, 1 to 2 teaspoons (5-10 mL) before bed can quiet a nighttime cough. Important: Never give honey to children under 1 year old. It can cause botulism - a rare but dangerous illness.2. Dextromethorphan (DM)
This is the active ingredient in many OTC cough syrups like Robitussin DM. It doesn’t cure bronchitis, but it can slightly reduce cough frequency. A 2014 Cochrane review showed it lowers coughing by a small but measurable amount. Take 15-30 mg every 6-8 hours, not more than 120 mg in 24 hours.3. Fluids and Humidifiers
Drink plenty of water - at least 8-10 glasses a day. It thins mucus so it’s easier to clear. Use a cool-mist humidifier in your bedroom. Breathing moist air soothes irritated airways. You can also lean over a bowl of hot water with a towel over your head - just be careful not to burn yourself.4. Pain and Fever Relief
If you have a low-grade fever or body aches, use acetaminophen (Tylenol) or ibuprofen (Advil). Stick to the label. Don’t exceed 3,000 mg of acetaminophen a day if you have liver issues. Ibuprofen can irritate your stomach, so take it with food.5. Avoid Inhaled Bronchodilators - Unless You Wheeze
Some people think inhalers like albuterol help with bronchitis cough. They don’t - unless you’re wheezing. Studies show no benefit for non-wheezers. And if you use them unnecessarily, you risk tremors, rapid heartbeat, or anxiety. If you’re wheezing, talk to your doctor - you might have asthma or bronchospasm.6. Skip Guaifenesin (Mucinex)
This expectorant is supposed to loosen mucus. But the evidence is weak. Out of seven studies, only two showed any real benefit. It’s not harmful, but don’t expect miracles.What to Say to Your Doctor
If you go in with a cough, your doctor should be able to tell if it’s bronchitis without an X-ray or lab test. But if you feel pressured to get antibiotics, here’s what to say:- “I’ve had this cough for 10 days with no fever. I’ve read that antibiotics usually don’t help with bronchitis. Can we talk about what else might help?”
- “I know coughs can last weeks. I just want to make sure it’s not something else.”
- “I’d rather avoid antibiotics unless they’re really needed.”
When to Worry - Red Flags
Most cases of acute bronchitis clear up on their own. But call your doctor if you have:- Fever over 38°C (100.4°F)
- Shortness of breath or wheezing that gets worse
- Coughing up blood
- Cough lasting more than 3 weeks
- Weight loss, night sweats, or fatigue that doesn’t go away
Why This Matters Beyond Your Cough
Choosing not to take antibiotics for bronchitis isn’t just about you. It’s about protecting everyone. Antibiotic resistance isn’t a future threat - it’s happening now. Superbugs are spreading in hospitals, homes, and communities. Every time we use antibiotics when we don’t need them, we make it harder to treat infections like sepsis, pneumonia, or even a simple cut that turns infected. The Choosing Wisely campaign, backed by medical societies across the U.S., says clearly: “Don’t prescribe antibiotics for acute bronchitis.” And the CDC, the American Academy of Family Physicians, and the American College of Chest Physicians all agree. The goal isn’t to make you suffer. It’s to help you heal - safely, effectively, and without adding to a growing public health crisis.What’s Coming Next?
Researchers are looking for better ways to tell viral from bacterial bronchitis. Right now, it’s mostly guesswork based on symptoms. But new studies - like the NIH-funded BREATHE trial - are testing natural remedies like ivy leaf extract. Early results are promising. The American Academy of Family Physicians also wants to cut inappropriate antibiotic prescribing for bronchitis to under 20% by 2026. That means better education, better tools, and better conversations between patients and doctors. Until then, the best thing you can do is rest, hydrate, use honey or dextromethorphan if needed, and resist the urge to reach for antibiotics. Your cough will fade. Your lungs will heal. And you’ll help save antibiotics for when they truly matter.Is acute bronchitis contagious?
Yes, the viruses that cause acute bronchitis are contagious - usually spread through coughs and sneezes. But once you’re sick, you’re not spreading the bronchitis itself. You’re spreading the virus. That’s why handwashing and covering your mouth when you cough matter. Most people stop being contagious after a few days, even if the cough lasts longer.
Can I get bronchitis more than once a year?
Yes. People who smoke, have asthma, or are frequently exposed to irritants like smoke or pollution are more likely to get bronchitis repeatedly. If you’ve had three or more episodes in a year, talk to your doctor. You might have a chronic condition like asthma or early COPD.
Does smoking make bronchitis worse?
Absolutely. Smoking damages your airways and slows healing. If you smoke and get bronchitis, your cough will last longer, you’ll be more likely to get it again, and your risk of developing chronic bronchitis or COPD increases dramatically. Quitting is the best thing you can do for your lungs - even after you’ve had bronchitis.
Should I use a cough suppressant or an expectorant?
It depends on your cough. If your cough is dry and keeps you awake, try a suppressant like dextromethorphan. If you’re coughing up thick mucus and feel like you can’t clear your chest, an expectorant like guaifenesin might help - but don’t expect it to work miracles. Honey often works better than either for nighttime coughs.
Can children get acute bronchitis?
Yes, but it’s less common in healthy children than in adults. When kids get it, the same rules apply: no antibiotics unless there’s clear evidence of bacteria. Honey is safe for kids over 1 year old and often works better than OTC cough syrups. Never give children under 4 any over-the-counter cough or cold medicine - it’s risky and often ineffective.

swati Thounaojam
January 8, 2026 AT 18:38My cough lasted 3 weeks last winter and my doctor didn’t even offer antibiotics. Just honey and rest. Worked fine.
Donny Airlangga
January 10, 2026 AT 15:19I used to panic every time I coughed for more than a week. Then I read this and realized I’d been taking antibiotics like candy. I haven’t taken one in over a year. My gut thanks me.
Annette Robinson
January 11, 2026 AT 11:36This is the kind of post that makes me believe in the internet again. So many people don’t realize how dangerous overprescribing is-not just for them, but for everyone. I’m a nurse and I see the fallout every day: kids with C. diff from antibiotics they never needed, elderly patients with resistant infections because the first line of defense was already useless. Thank you for laying this out so clearly. Honey really does work better than syrup. I give it to my nieces every time they get a cold.
Kristina Felixita
January 11, 2026 AT 15:13OMG YES!! I’ve been telling my mom for YEARS not to ask for antibiotics for every sniffle-she still does it tho 😭 I printed this out and gave it to her. She cried and said she never knew about the resistance thing. Now she uses honey and steam and even lets me read her the part about dextromethorphan. She’s 68 and still stubborn but she’s trying!!
christy lianto
January 12, 2026 AT 20:13I used to think if I didn’t get antibiotics, I wasn’t being taken seriously. I’d sit there, sweating through my shirt, coughing into a tissue, and beg for a script. Then I got a doctor who didn’t blink. Said, ‘You’re not sick enough to need this, but you’re sick enough to need sleep.’ I cried. Not from sadness-from relief. I hadn’t realized how much I’d been conditioned to think medicine = pills. Turns out, rest, water, and time are the real magic. I’ve had two bronchitis episodes since. No antibiotics. Both gone in 18 days. I’m not scared anymore.
Aubrey Mallory
January 12, 2026 AT 23:38Stop letting pharmaceutical companies dictate your health choices. You think they care that you’re coughing? No. They care that you’re buying their pills. This post is the truth wrapped in science-not opinion. And if your doctor still prescribes antibiotics for bronchitis, find a new one. That’s not medical care, it’s negligence dressed up as convenience. We’re not talking about minor side effects here-we’re talking about a global health emergency. Wake up.
Ken Porter
January 13, 2026 AT 07:54Why are we even having this conversation? In my country, we don’t waste time with honey and humidifiers. We treat it fast-antibiotics, done. You think the U.S. is the only place that matters? Your ‘evidence-based’ nonsense is why we’re falling behind in global health outcomes. Just give people what works.
Lois Li
January 13, 2026 AT 12:13Ken, I hear you-but you’re mixing up speed with effectiveness. In countries where antibiotics are overused, we’re seeing more treatment failures, longer recoveries, and higher death rates from infections that used to be easy to cure. The WHO says antibiotic resistance could kill 10 million a year by 2050 if we don’t change. That’s not ‘falling behind’-that’s walking into a wall. I’ve worked in public health in three countries. The places that resisted overprescribing? Their ERs are calmer, their kids are healthier, and their antibiotics still work. This isn’t American privilege. It’s survival.